5 Signs How to Know Eye Infections – Ignore Them Not!
“Discover the Crucial Signs of Eye Infections in Our Current Post! Learn How to Recognize Symptoms Early, and Why Ignoring them Is Not an Option. Protect Your Vision with Essential Insights on Eye Health.”
Introduction
Welcome to our insightful guide on recognizing and addressing eye infections. In an era where our screen time is on the rise, prioritizing eye health is more crucial than ever.
Titled ‘5 Signs How to Know Eye Infections – Ignore Them Not!’ this post emphasizes the immediate attention eye infections demand.
Eye infections, if overlooked, can lead to permanent damage, impacting your eyesight for a lifetime. The consequences are too significant to ignore.
This blog post sheds light on the five most common signs of an eye infection and emphasizes the critical importance of seeking prompt medical attention if you experience any of these indicators.
Don’t take chances with your vision—discover the key signs and why ignoring them is not an option in our comprehensive exploration of eye infections.
Disclosure
Before delving further into the content, it’s essential to establish a foundation of clarity and transparency.
It’s worth noting that this post might be enriched with affiliate links, which serve as a means to sustain the quality of this platform.
These links come with a distinct advantage – they grant me a modest commission, a portion that comes directly from the seller and doesn’t include any additional costs on your end.
Intriguingly, some of these links also offer you a noteworthy benefit: exclusive discounts that are accessible through these very channels. It’s a win-win scenario.
By clicking and making purchases via these links, you extend your support toward the continuous upkeep and enhancement of this blog.
Your actions foster the creation of genuine, insightful content that’s dedicated to your enrichment.
It’s imperative to emphasize that I find genuine satisfaction in endorsing tools and resources that I hold dear, employ regularly, and have personally vetted.
This ensures that the content I present is not only reliable but also backed by firsthand experience.
As you immerse yourself in the post, my sincere hope is that it serves you in meaningful ways. May it contribute to your knowledge reservoir or introduce you to new insights.
Your commitment is genuinely appreciated.
Wishing you an enlightening reading experience ahead!
I – Common Types of Eye Infections
Common Types of Eye Infections: Unveiling Ocular Health Challenges
In this section, we’ll explore various eye infections that pose potential threats to ocular health.
From the well-known conjunctivitis to the less familiar keratitis, we’ll unravel the characteristics, causes, and treatment options for these common eye ailments.
Let’s navigate through the diverse landscape of eye infections to empower you with knowledge about safeguarding your eyesight.
A – Conjunctivitis (Pink Eye)
01 – Symptoms
Conjunctivitis, commonly known as Pink Eye, manifests through noticeable symptoms that signal an eye infection.
Watch for redness, itching, and a gritty sensation in the eye. Excessive tearing and discharge, often causing eyelids to stick together, are common indicators.
Additionally, heightened sensitivity to light might accompany pink eye.
02 – Causes
Understanding the causes is key to preventing and managing conjunctivitis.
It can result from viral or bacterial infections, allergies, or irritants like smoke and pollutants.
Identifying the specific cause helps determine the most effective course of treatment.
03 – Treatment Options
Treatment for conjunctivitis varies based on its cause. Viral conjunctivitis often resolves on its own, with supportive care like cool compresses.
Bacterial conjunctivitis may require antibiotics, while allergic conjunctivitis benefits from antihistamines.
Consulting with an eye care professional ensures accurate diagnosis and appropriate treatment, fostering a speedy recovery.
A1 – Allergic Conjunctivitis
01 – Symptoms
Allergic conjunctivitis triggers specific symptoms that distinguish it from other types of eye conditions.
This range of uncomfortable symptoms includes red, itchy eyes, often accompanied by excessive tearing. Swelling of the eyelids, the feeling of grittiness in the eye, and a burning sensation are also common discomforts.
In some cases, individuals may experience sensitivity to light.
People with a history of allergies or asthma are at a higher risk of developing allergic conjunctivitis.
02 – Causes
Allergic Conjunctivitis is a type of eye inflammation that occurs when the Conjunctiva – the thin layer of tissue that covers the white part of the eye and inner surface of the eyelids -, comes into contact with an allergen.
Common allergens that trigger allergic conjunctivitis include pollen, dust mites, pet dander, and mold.
When these allergens enter the eye, they trigger the release of histamines, which cause the blood vessels in the conjunctiva to dilate and become inflamed.
03 – Treatment Options
Managing allergic conjunctivitis involves both prevention and treatment.
Avoiding exposure to allergens is the first line of defense. Proper diagnosis and treatment by an eye doctor, are mostly advised.
The doctor may prescribe medications including antihistamine eye drops or oral medications, which will provide relief by alleviating itching and redness, helping to manage the symptoms and prevent complications.
Cold compresses may also soothe irritation. Consultation with an eye care professional is advisable for a tailored approach to address individual symptoms and triggers effectively.
A2 – Bacterial Conjunctivitis
01 – Symptoms
Bacterial conjunctivitis exhibits distinct symptoms that signal a bacterial infection in the eye.
The symptoms of Bacterial Conjunctivitis typically include redness, swelling, itching, and a yellow or green discharge from the eye. In some cases, the eyelids may stick together or crust over during sleep.
Individuals with bacterial conjunctivitis may experience a gritty or sticky feeling in the eyes. Crustiness, particularly upon waking, is also a common symptom.
02 – Causes
Bacterial Conjunctivitis is highly contagious and can be spread through direct contact with an infected person’s eye discharge, or by sharing contaminated items like towels, eye makeup, or contact lenses.
The most common bacterial strains that cause this infection include Staphylococcus Aureus, Streptococcus Pneumonia, and Haemophilus Influenza.
The bacteria can spread through direct contact with an infected person, touching contaminated surfaces, or from other existing infections, such as sinus or ear infections.
03 – Treatment Options
Treating bacterial conjunctivitis typically involves antibiotics, either in the form of eye drops or ointments.
It’s essential to complete the full course of antibiotics as prescribed by a healthcare professional to ensure the complete elimination of the infection.
Applying warm compresses can also alleviate discomfort and aid in the recovery process. If you suspect bacterial conjunctivitis, seek prompt medical attention for accurate diagnosis and appropriate treatment.
A3 – Viral Conjunctivitis
01 – Symptoms
Viral conjunctivitis, often associated with common viral infections, manifests with specific symptoms.
The symptoms typically include redness, irritation, swelling, itching, and a watery discharge from the eye. In some cases, the eyelids may become sensitive to light.
Individuals may experience a sensation of grittiness or discomfort. Unlike bacterial conjunctivitis, the discharge in viral cases tends to be clear or watery.
02 – Causes
Viral Conjunctivitis is a highly contagious eye infection caused by a virus that infects the Conjunctiva.
Viral conjunctivitis is primarily caused by viruses such as adenoviruses, which are responsible for various respiratory infections.
Viruses such as Herpes Simplex Virus, and Varicella-zoster Virus are also responsible for Viral conjunctiva.
It can spread through direct contact with infected individuals’ eye discharge or by touching contaminated objects, like towels or doorknobs.
People who have weakened immune systems or who have had recent exposure to someone with Viral Conjunctivitis are at a higher risk of developing the infection.
Being vigilant about personal hygiene and avoiding contact with infected persons can help prevent its transmission.
03 – Treatment Options
Unlike bacterial conjunctivitis, viral conjunctivitis typically does not respond to antibiotics. Antiviral medications may be prescribed by an eye doctor to help manage the symptoms and prevent complications
Treatment focuses on relieving symptoms and letting the infection run its course. Cold compresses can soothe irritation, and over-the-counter lubricating eye drops may provide relief.
It’s crucial to consult with a healthcare professional for an accurate diagnosis and appropriate guidance on symptom management during the healing process.
Proper hygiene practices like washing hands frequently and avoiding sharing personal items can also help prevent the spread of Viral Conjunctivitis.
B – Blepharitis
01 – Symptoms
Blepharitis is a common eye condition that occurs when the Oil Glands in the eyelids become inflamed and clogged. It presents itself with noticeable symptoms affecting the eyelids.
Common signs include red and swollen eyelids, flaky or crusty skin around the base of the eyelashes, itching, and a feeling of burning or grittiness.
Individuals with Blepharitis may also experience greasy eyelashes, and in severe cases, Blepharitis can also lead to blurred vision or sensitivity to light.
02 – Causes
Several factors contribute to the development of blepharitis. It can be linked to bacterial overgrowth on the eyelids, issues with the oil glands in the eyelids, or conditions like seborrheic dermatitis.
Poor eyelid hygiene, allergies, and certain systemic conditions may also play a role.
03 – Treatment Options
Managing blepharitis involves a combination of good eyelid hygiene and targeted treatments.
Warm compresses can help soften crusts, and gentle cleaning of the eyelids with a mild soap or prescribed eyelid cleanser is recommended. In some cases, antibiotic ointments or steroid eye drops may be prescribed.
Consistent eyelid hygiene practices and regular eye examinations can contribute to effectively managing and preventing the recurrence of blepharitis symptoms.
If you suspect Blepharitis, consulting with an eye care professional is advisable for personalized guidance.
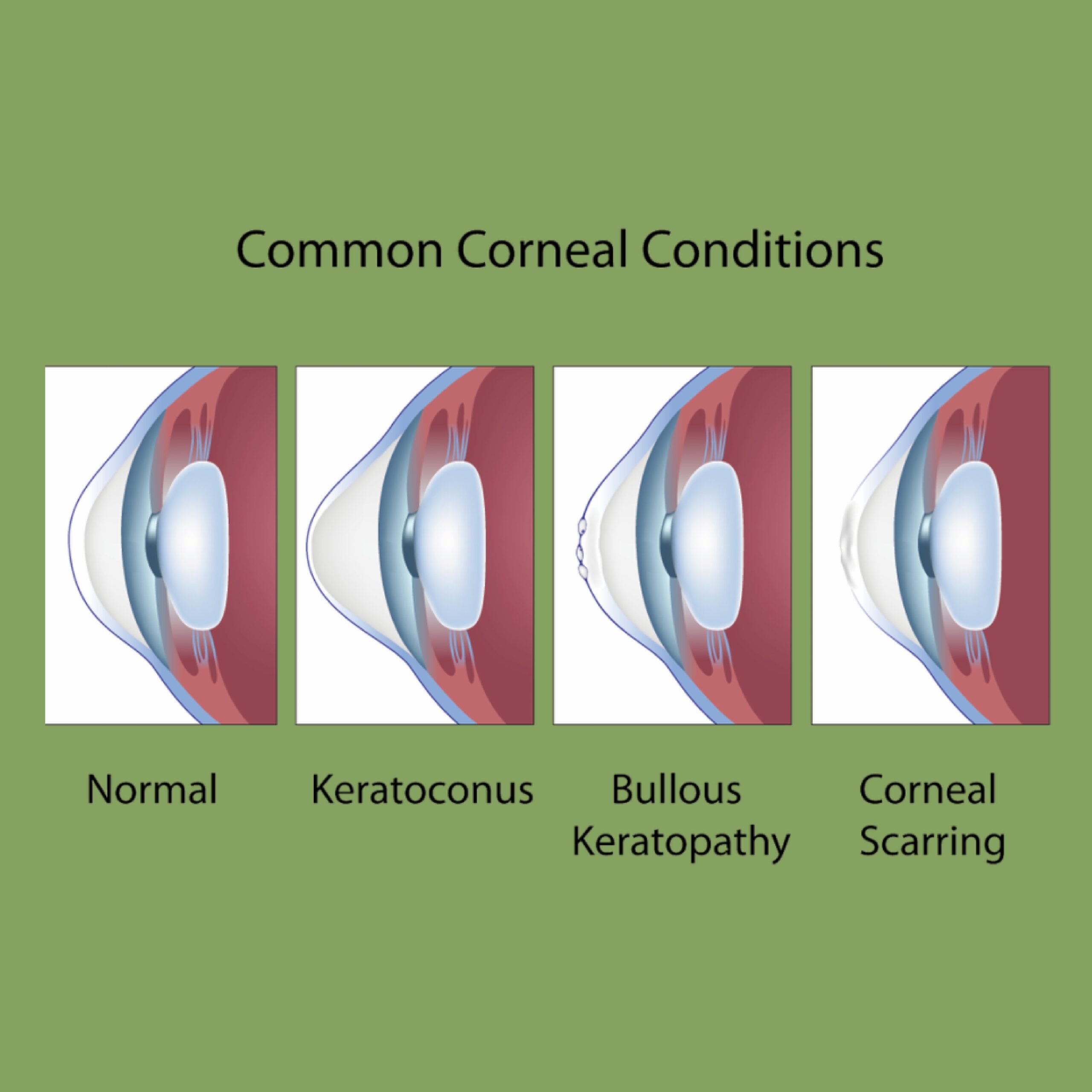
C – Keratitis
01 – Causes and Risk Factors
Keratitis, the inflammation of the cornea, can be caused by a variety of factors, including bacterial, viral, fungal, or parasitic infections, as well as exposure to environmental irritants or trauma to the eye.
Contact lens wearers face an increased risk, especially if lenses are not cleaned properly.
Other risk factors may include eye injuries, dry eyes, and certain pre-existing conditions like autoimmune diseases.
02 – Symptoms
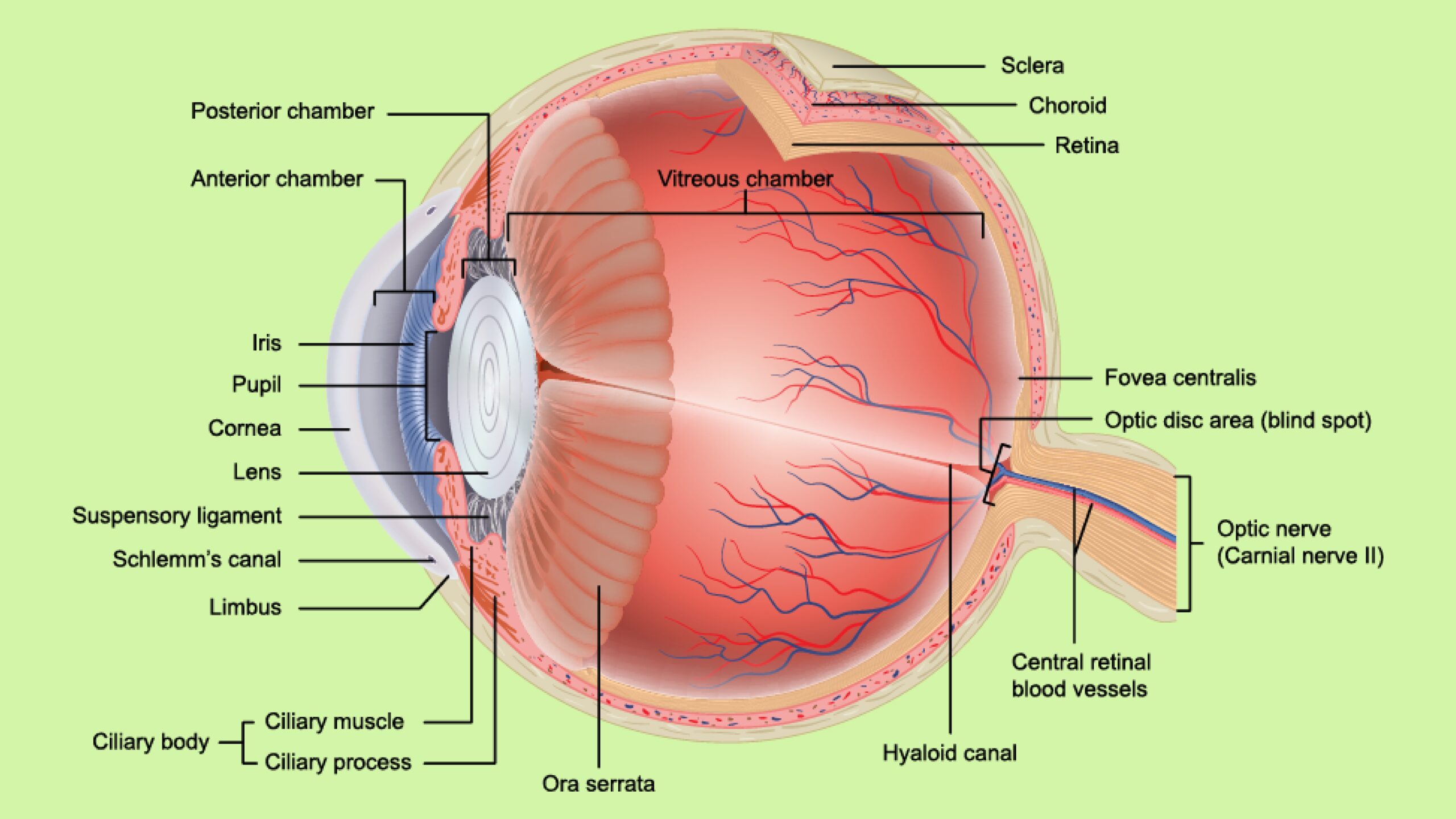
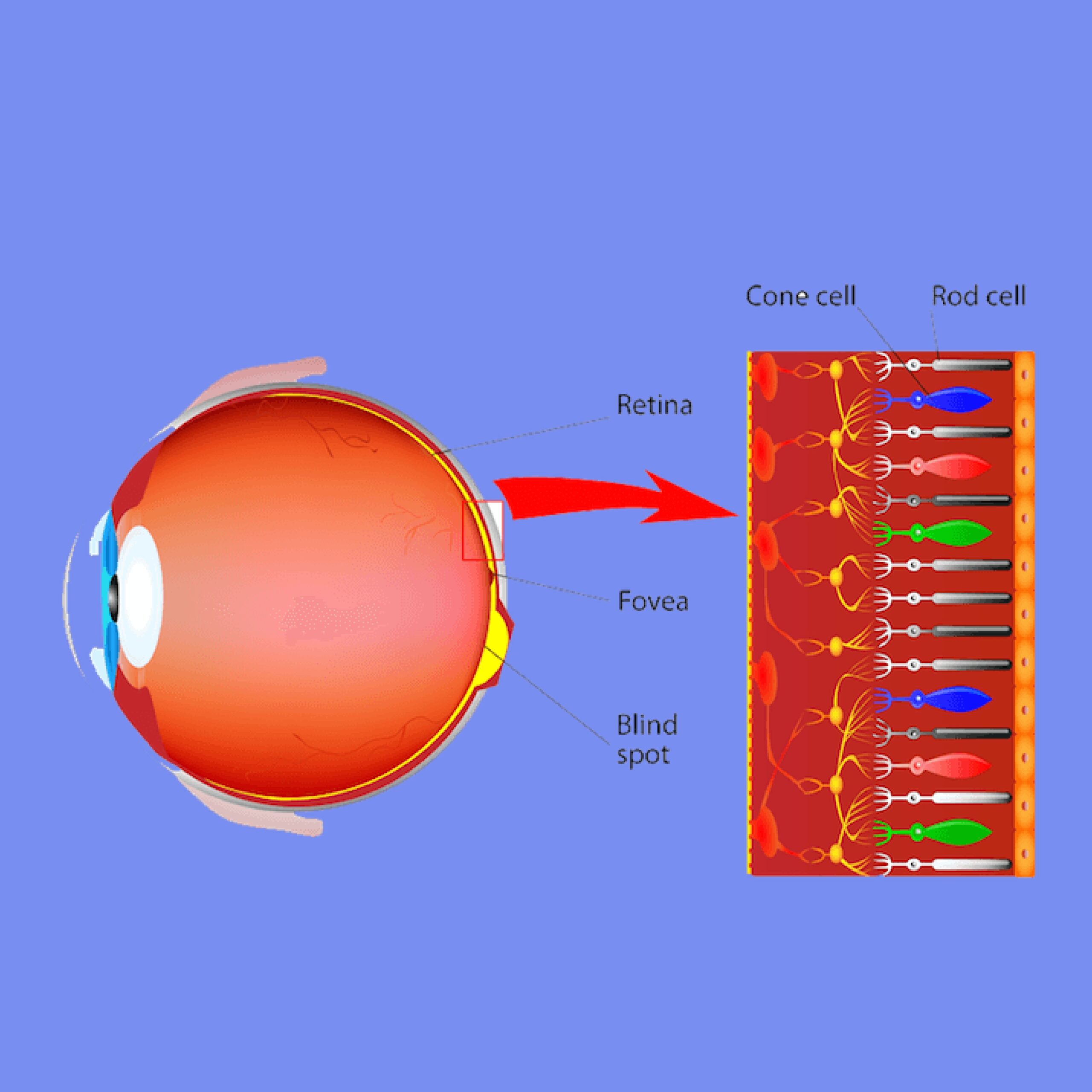
Keratitis is a condition characterized by inflammation of the cornea, the clear outer covering of the eye that helps focus light onto the retina.
The symptoms of Keratitis may vary depending on the underlying cause, and recognizing these symptoms is crucial for early intervention.
Individuals may experience eye redness, pain, heightened sensitivity to light blurred or hazy vision, the feeling of a foreign body in the eye, and excessive tearing.
In severe cases, Keratitis can lead to scarring of the cornea or vision loss. Prompt attention to these symptoms is essential for preventing complications.
03 – Treatment Approaches
Treatment for Keratitis depends on the underlying cause. It may include the use of antibiotic or antifungal medications, steroids, or corticosteroid eye drops to reduce inflammation.
Bacterial keratitis often requires antibiotics, while antiviral medications may be prescribed for viral forms.
Fungal keratitis may need antifungal medications.
In severe cases, hospitalization might be necessary for surgery to remove damaged tissue.
Good hygiene practices, such as washing hands frequently and avoiding touching the eyes, can help reduce the risk of developing Keratitis.
Seeking immediate medical attention is crucial for accurate diagnosis and appropriate treatment to preserve vision and prevent complications.
D – Stye
01 – Identifying a Stye
Identifying a Stye involves recognizing a small, red bump on the eyelid resembling a pimple. It’s usually painful and may be accompanied by swelling.
Styes often develop near the eyelash line and can involve the upper or lower eyelid. While they are typically harmless, knowing how to differentiate a stye from other eye issues is crucial for appropriate management.
02 – Home Remedies and Medical Treatments
For at-home relief, warm compresses applied to the affected eye can help reduce pain and encourage the stye to drain.
Avoid squeezing or attempting to pop a stye, as this can lead to further complications. Over-the-counter pain relievers can be used to manage discomfort.
Medical treatments may be necessary if the stye persists or worsens. A healthcare professional may recommend antibiotic ointments or oral antibiotics to address bacterial infection.
In some cases, minor surgical procedures may be considered to drain the stye. Seeking professional advice ensures proper diagnosis and the most suitable treatment plan for effective and safe resolution.
II – 5 Signs of Possible Eye Infections
5 Signs of Possible Eye Infections: A Guide to Early Recognition
In this section, we’ll explore five key signs that may indicate the presence of eye infections. Recognizing these indicators early is crucial for timely intervention and maintaining optimal eye health.
Whether you’re experiencing redness, irritation, changes in vision, or other symptoms, understanding these signs empowers you to take proactive steps toward seeking the appropriate care.
Let’s start unraveling the telltale signs that should never be ignored when it comes to your eye health.
A – Redness and Irritation
01 – What to Look For
When it comes to redness and irritation, pay attention to noticeable changes in the color of your eyes. If your eyes appear more red than usual and feel itchy or uncomfortable, it could indicate an issue.
Itching of the eyelids or eyes is a very common symptom that can be caused by a wide range of factors.
It can feel like a persistent urge to rub your eyes or a tickling sensation that just won’t go away.
Itching can occur due to various reasons such as allergies, infections, or even dry eyes.
There are several reasons why you may experience discomfort in your eyes, including infections, allergies, or injury.
Additionally, be on the lookout for any swelling or a sensation of grittiness, as these are common signs associated with redness and irritation.
02 – When to Seek Medical Attention
While occasional redness may result from factors like fatigue or dryness, persistent redness accompanied by pain or worsening symptoms warrants immediate attention.
If over-the-counter remedies provide no relief or if redness is accompanied by other concerning signs, such as discharge or changes in vision, it’s crucial to seek prompt medical attention.
Professional evaluation ensures an accurate diagnosis and appropriate treatment to address the underlying cause of redness and irritation effectively.
B – Excessive Tearing
01 – Understanding Normal Tear Production
Tears play a vital role in maintaining eye health by keeping the eyes lubricated and protecting against irritants. Normal tear production is a balanced process, with tears constantly being produced and drained away.
This delicate equilibrium ensures comfort and clear vision. Understanding what constitutes normal tear production involves recognizing when tears serve their protective function without causing excessive tearing.
02 – When Tearing Becomes a Concern
Excessive tearing, or epiphora, occurs when there is an imbalance in tear production or drainage. If you find yourself frequently tearing up without an apparent reason, it may signal an underlying issue.
Factors such as irritation, allergies, or blockages in the tear ducts can contribute to excessive tearing.
If this symptom persists or is accompanied by other discomforts like redness or vision changes, it’s advisable to consult with a healthcare professional.
Identifying the root cause is crucial for appropriate management and ensuring that your eyes stay comfortable and healthy.
C – Sensitivity to Light
01 – Exploring Photophobia
Photophobia, or sensitivity to light, refers to an increased sensitivity or discomfort when exposed to light. This condition can make even normal levels of light feel intense and bothersome.
Exploring Photophobia involves recognizing the situations and environments where this sensitivity arises, along with understanding its impact on daily activities.
02 – Connection to Eye Infections
Sensitivity to light can be linked to various eye conditions, including infections. Eye infections may cause inflammation, making the eyes more sensitive to light.
If you find yourself squinting or avoiding bright lights due to discomfort, it could be a sign of an underlying eye infection.
Considering the connection between sensitivity to light and eye infections is crucial for identifying potential issues early on.
If this sensitivity persists or is accompanied by other symptoms, seeking professional evaluation ensures accurate diagnosis and appropriate treatment to alleviate discomfort and address the underlying cause.
D – Discharge from the Eye
01 – Types of Discharge
Discharge from the eye can take various forms, including watery, thick, yellow, or green. Understanding these different types of discharge involves paying attention to the consistency and color.
Clear and watery discharge may be normal, especially if it’s a response to irritation. However, thicker or colored discharge can indicate an underlying issue, such as an infection.
02 – Significance in Differentiating Infections
The type of eye discharge holds significance in differentiating between various eye conditions, especially infections.
Bacterial infections often produce thick, yellow, or green discharge, while viral infections may result in a watery discharge.
Recognizing these distinctions is crucial for early identification and appropriate treatment.
If you observe unusual or persistent discharge, especially if it’s accompanied by other symptoms like redness or discomfort, seeking professional guidance ensures an accurate diagnosis and effective management of the underlying issue.
E – Changes in Vision
01 – Blurriness and Other Vision Changes
Changes in vision, such as blurriness, difficulty focusing, or sudden visual disturbances, can be warning signs of underlying issues.
The blurring of vision is a concerning symptom that can be indicative of a wide range of eye conditions.
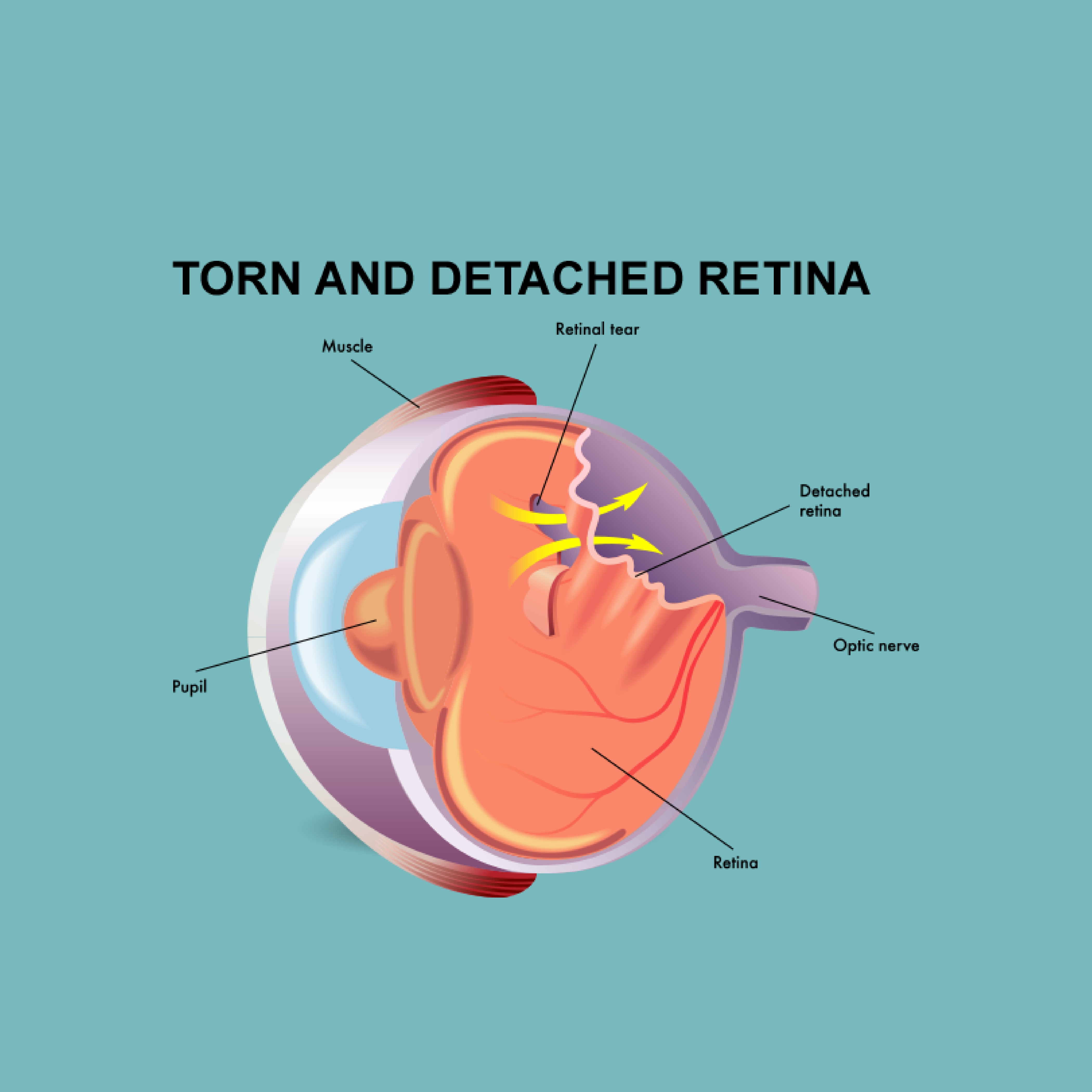
Blurring of vision can occur due to reasons such as cataracts, macular degeneration, or retinal detachment.
In some cases, blurring of vision may also be accompanied by other symptoms such as flashes of light, floaters, or double vision.
Understanding these vision changes involves recognizing when your sight deviates from your normal visual experience. It’s important to pay attention to any alterations in clarity or sharpness, as well as the onset of new visual symptoms.
02 – Immediate Action Steps
If you notice sudden changes in your vision or experience any sudden or gradual blurring of your vision, taking immediate action is crucial. It’s therefore, essential to contact your eye doctor immediately.
Ignoring these symptoms can lead to more severe complications that can affect your ability to see clearly and potentially cause permanent vision loss.
Addressing vision changes promptly involves scheduling an eye examination with a healthcare professional.
Delaying assessment may contribute to complications. If you experience persistent blurriness, distorted vision, or other unusual changes, seek professional advice promptly.
Early intervention not only helps identify potential issues but also ensures timely and appropriate measures to preserve your eye health and maintain clear vision.
Don’t overlook any changes in your vision; it’s always better to be safe than later say sorry when it comes to your eyesight.
Your eye doctor is qualified to perform a comprehensive eye exam to diagnose the underlying cause of your blurring vision and recommend the most appropriate treatment plan.
III – Eye Infections, Eye Diseases, and Vision Disorders
Our intricate and fragile eyes are vulnerable to a diverse array of diseases and infections.
These conditions do not discriminate based on age and can be instigated by various factors, encompassing bacteria, viruses, fungi (fungus), parasites, and environmental irritants.
Symptoms of eye diseases and infections manifest in various ways, ranging from redness and pain to discharge, sensitivity to light, blurred vision, and, in severe cases, vision loss.
Below, we provide insights into both well-known and less common eye diseases and infections, aiming to enhance awareness and understanding of these critical issues.
A – Amblyopia
Amblyopia, commonly known as Lazy Eye, is a condition in which one eye experiences diminished vision compared to the other, despite the affected eye itself being structurally sound.
This condition arises when the brain and the eye fail to synchronize effectively, leading the brain to rely more on the ‘stronger’ eye.
Typically emerging in early childhood, Amblyopia can stem from various causes, including:
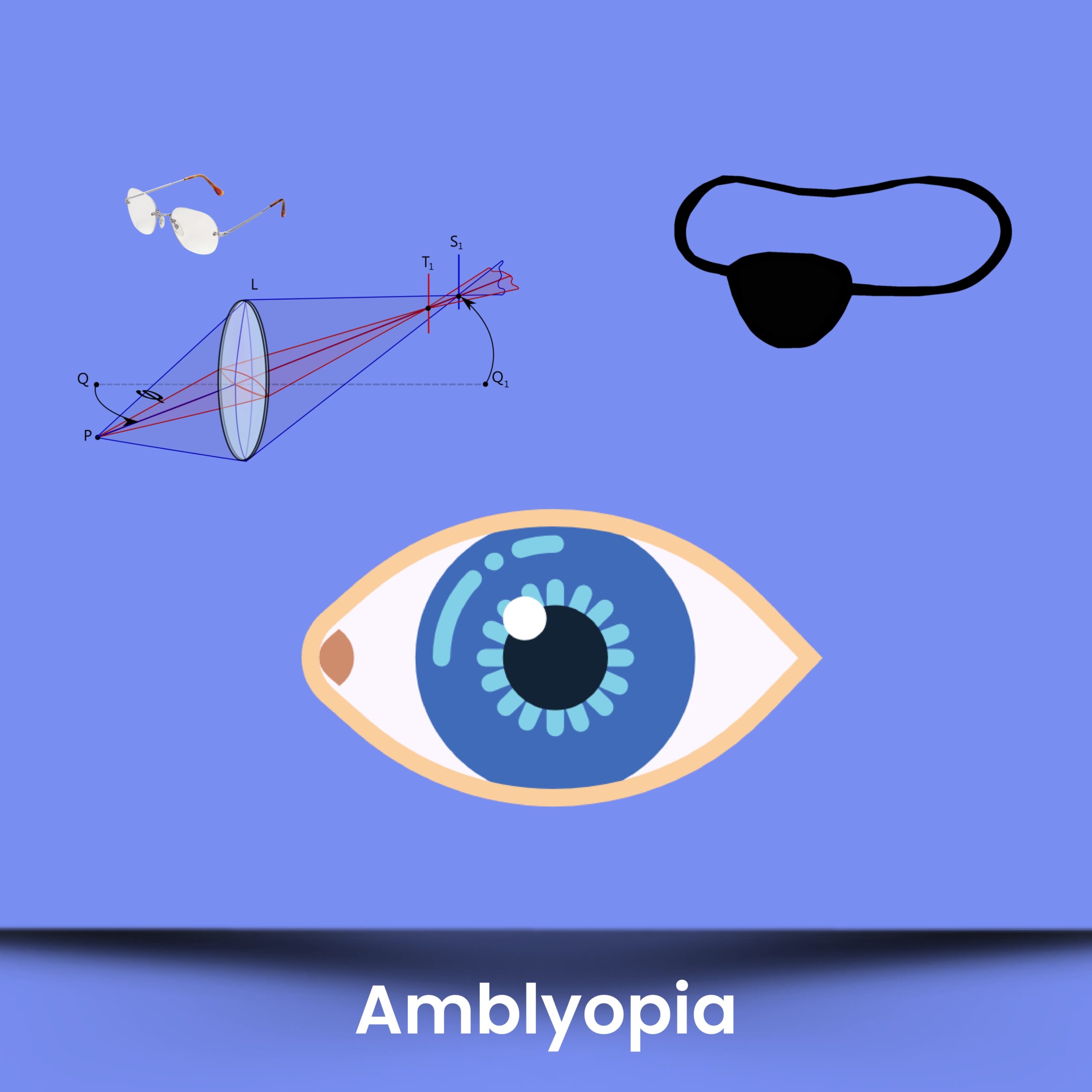
Strabismus: Misalignment of the eyes.
Anisometropia: A discrepancy in the refractive power of the eyes.
Deprivation: Obstruction of clear visual images to one eye, often due to conditions like cataracts.
Prompt treatment of Amblyopia is essential to prevent permanent vision loss in the affected eye.
The treatment approach typically involves addressing the root causes, which may include the use of corrective glasses to rectify refractive errors or patching the stronger eye to encourage the brain to rely more on the weaker one.
Additionally, vision therapy may be recommended to enhance coordination between the eyes and the brain.
Early detection and intervention play a crucial role in achieving the best possible outcome for Amblyopia.
Regular eye examinations for children are strongly recommended to monitor their vision and identify potential issues at an early stage.
B – Ametropia
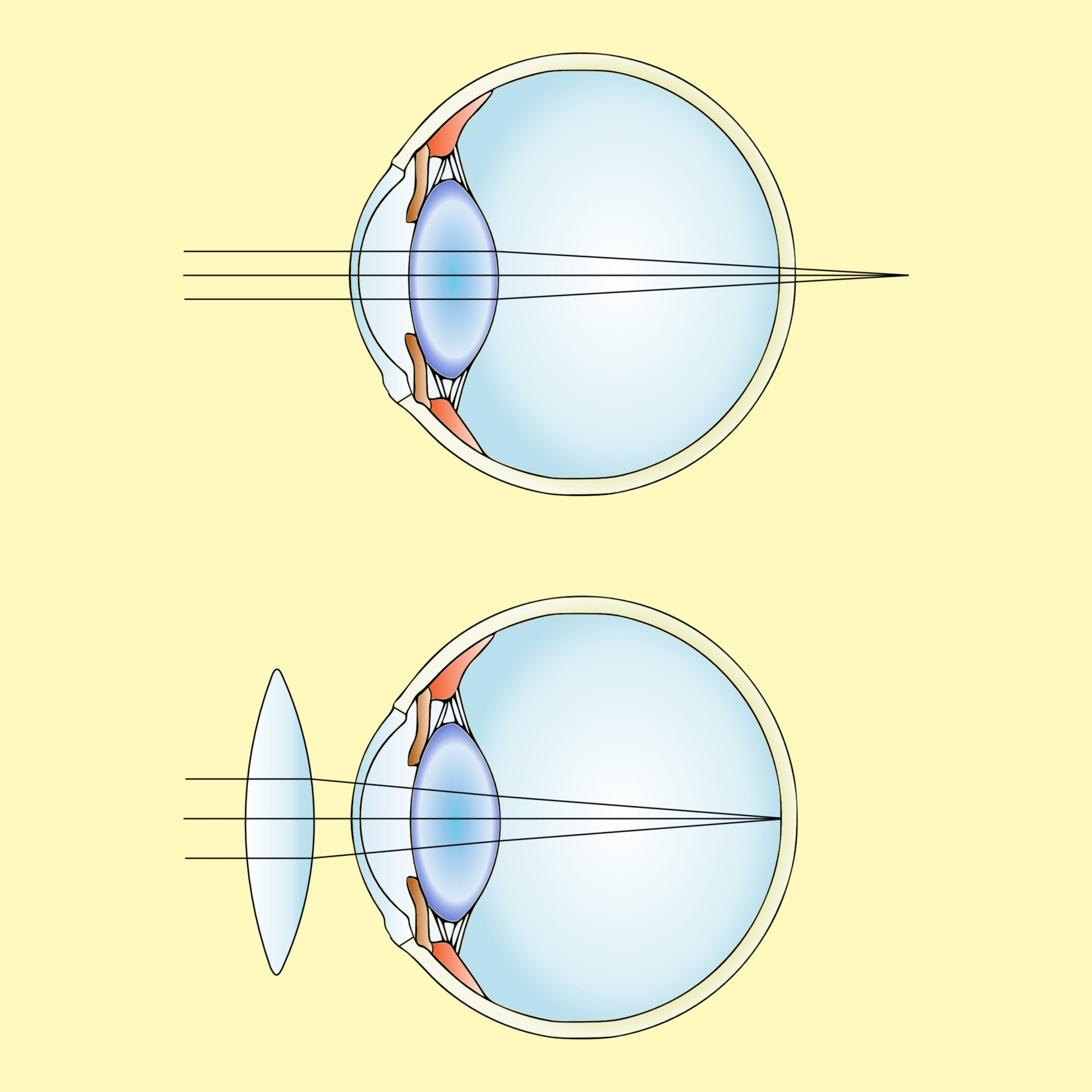
Ametropia, a medical term denoting an eye condition causing a refractive error, signifies the eye’s inability to properly focus light onto the retina, resulting in blurred or distorted vision.
Three primary types of Ametropia include Myopia, Hyperopia, and Astigmatism.
Each is detailed individually below.
Myopia: Commonly known as nearsightedness, where distant objects appear blurry.
Hyperopia: Also known as farsightedness, causing close-up objects to be less clear.
Astigmatism: Characterized by distorted vision due to irregular curvature of the cornea or lens.
Corrective measures for Ametropia include eyeglasses, contact lenses, or refractive surgery.
Regular eye exams play a pivotal role in identifying and managing refractive errors, while also monitoring for the potential development of other eye conditions over time. Proactive eye care ensures optimal visual health and well-being.
C – Astigmatism
Astigmatism arises when the cornea or lens of the eye assumes an irregular shape, causing light to converge at multiple points on the retina.
This condition leads to distorted or blurred vision across all distances.
While the precise causes of astigmatism remain not entirely understood, it is often associated with genetic factors and the inherent shape of the eye.
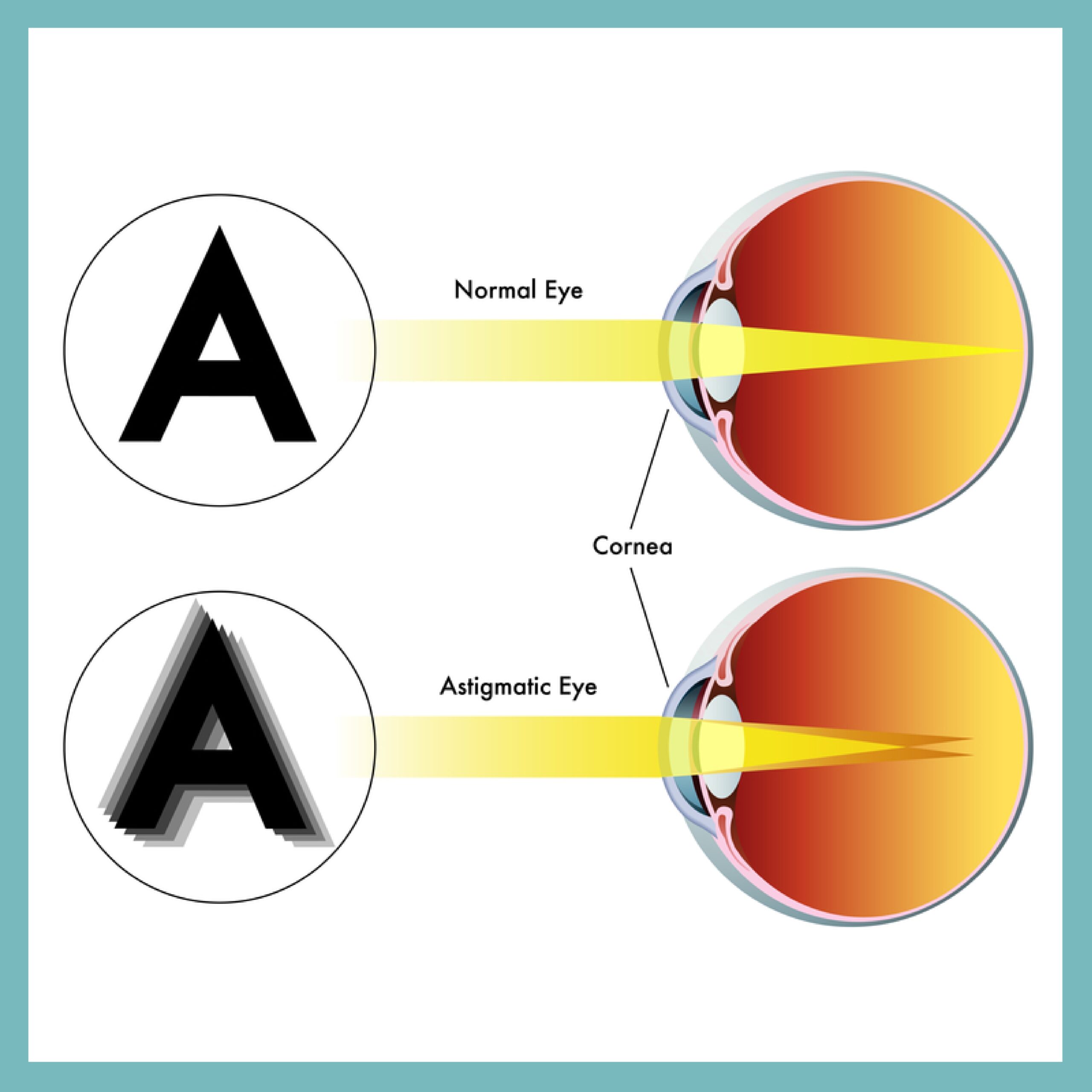
Onset can occur at any age, and risk factors include eye injury, surgery, or certain diseases.
Astigmatism may be present independently or in conjunction with nearsightedness or farsightedness.
Common symptoms encompass blurry or distorted vision, headaches, eye strain, and challenges seeing clearly at night.
Diagnosis is achieved through a comprehensive eye exam conducted by an optometrist or ophthalmologist.
Correction of astigmatism is typically accomplished through prescription eyeglasses or contact lenses, specially designed to compensate for the irregular corneal or lens shape.
In certain cases, refractive surgery options such as LASIK (Laser-Assisted in Situ Keratomileusis) or PRK (PhotoRefractive Keratectomy) might be recommended to reshape the cornea and enhance vision.
Individuals experiencing symptoms of blurry or distorted vision are encouraged to schedule an eye exam with an eye care professional.
This proactive step aids in determining the causes and identifying the most suitable course of treatment for optimal visual clarity.
D – Blepharitis
Blepharitis is a prevalent eye condition affecting the eyelids, characterized by symptoms like redness, itching, and irritation.
This condition arises when the oil glands at the base of the eyelashes become obstructed or infected, leading to inflammation.
Common signs of blepharitis include redness, swelling of the eyelids, itching or burning of the eyes, excessive tearing, and crusting or scaling of the eyelashes.

Blurred vision or light sensitivity may also be experienced by individuals with blepharitis.
Contributing factors to this condition include bacterial or fungal infections, allergies, and skin conditions like rosacea or seborrheic dermatitis.
Treatment for blepharitis involves a multifaceted approach, incorporating warm compresses, eyelid scrubs, and medicated eye drops or ointments to manage inflammation and infection.
In some instances, oral antibiotics or other medications may be prescribed to address underlying infections or skin conditions contributing to blepharitis.
Maintaining good eyelid hygiene and refraining from rubbing or scratching the eyes are essential practices to prevent symptom exacerbation.
With diligent care and proper management, most individuals with blepharitis can successfully control symptoms and safeguard their eyes from long-term damage.
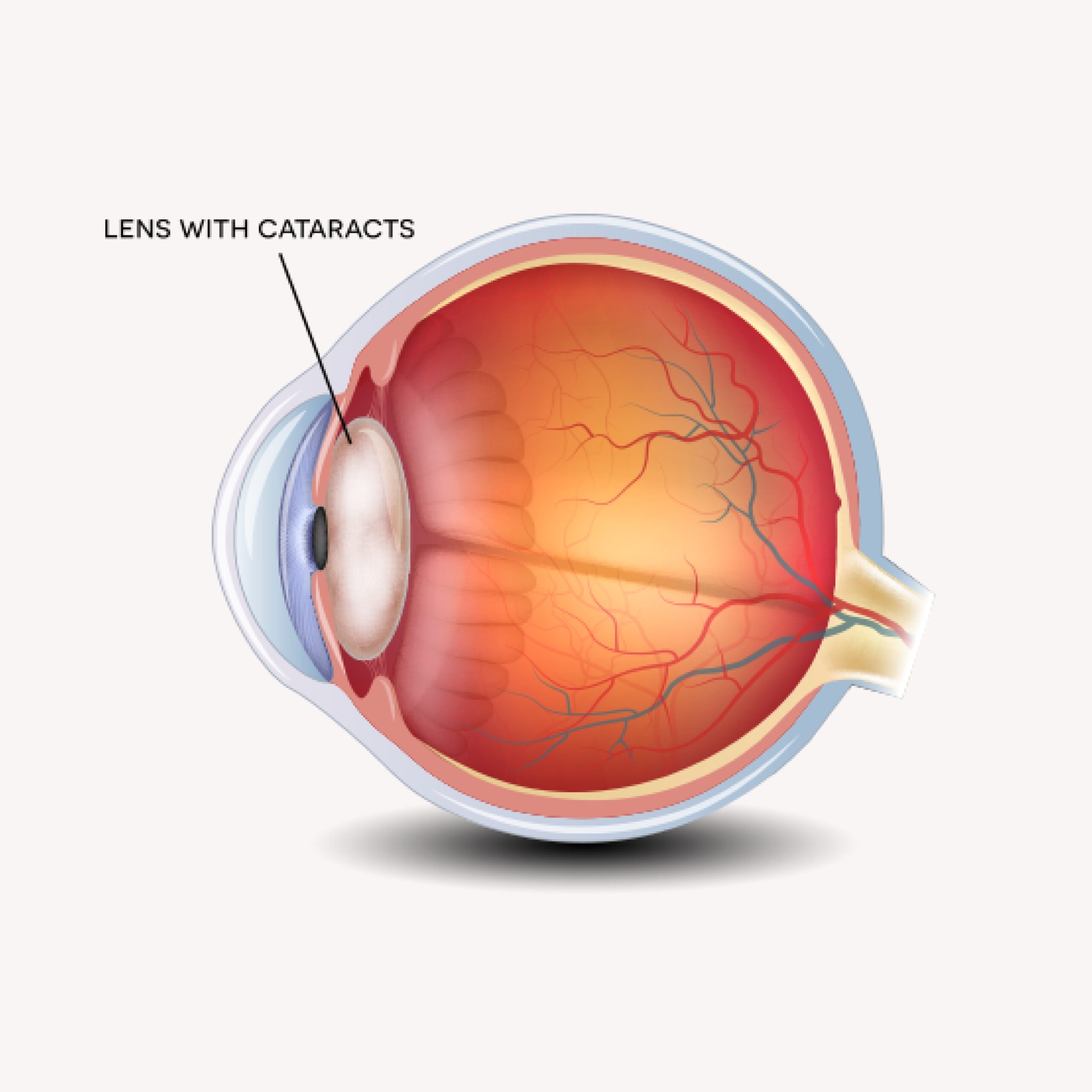
E – Cataract
Cataracts represent a clouding of the eye lens, a prevalent condition impacting the lens’s clarity within the eye.
Positioned behind the iris, the clear lens aids in focusing light onto the retina, the light-sensitive tissue at the eye’s back.
In the presence of cataracts, this lens becomes cloudy or opaque, resulting in blurred vision, sensitivity to glare, and challenges in seeing in dim light.
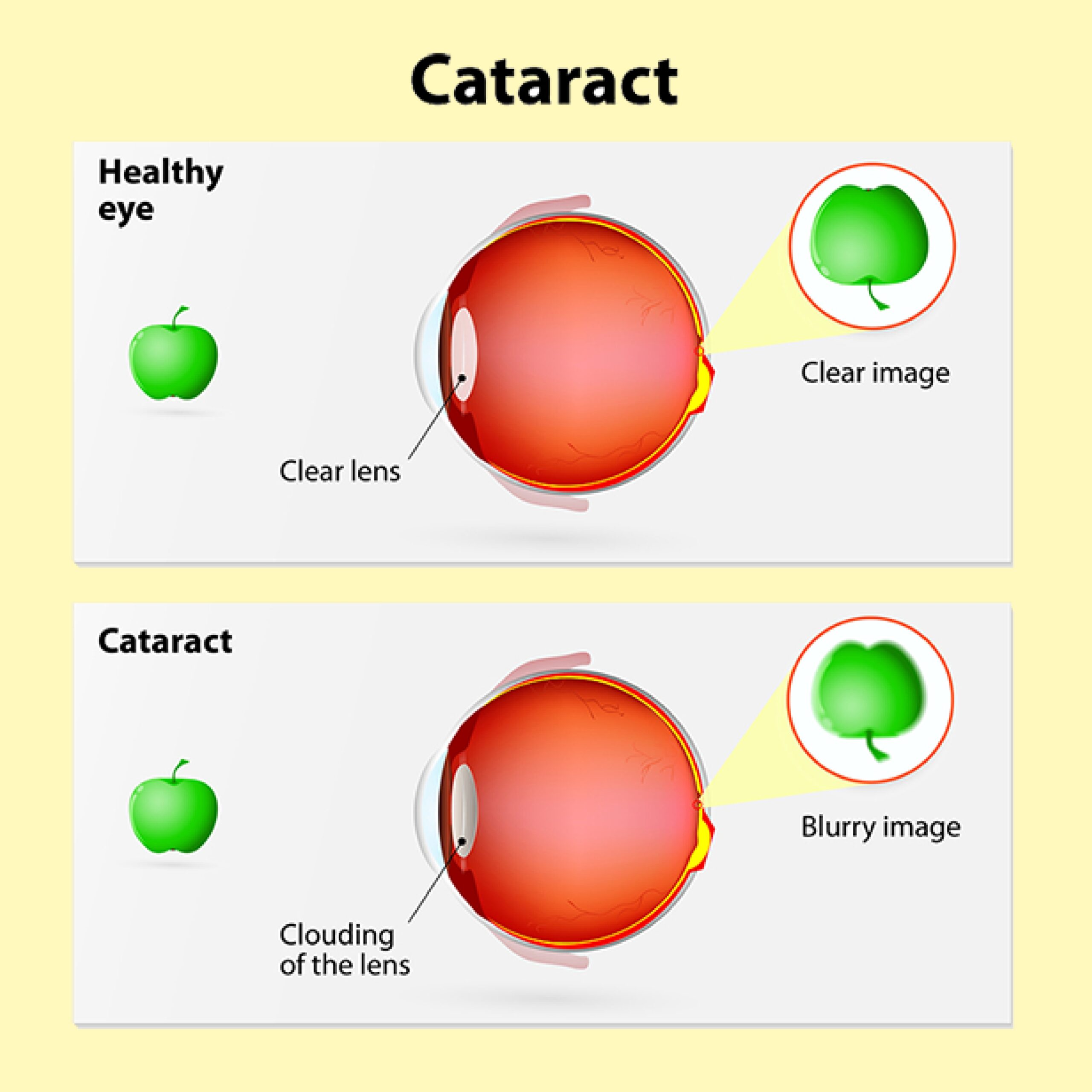
Colors may also appear less vivid, requiring frequent adjustments to eyeglasses or contact lens prescriptions.
A variety of factors can contribute to cataracts, including aging, genetics, certain medications, eye injuries, and medical conditions like diabetes.
The primary treatment for cataracts involves surgery, a safe and effective procedure where the cloudy lens is removed and replaced with an artificial lens known as an Intraocular Lens (IOL).
Cataract surgery boasts a high success rate and minimal risk of complications.
Early detection and timely treatment are paramount to preserving good vision and overall quality of life.
Regular eye exams are strongly recommended, especially for individuals over the age of 60 or those with a family history of cataracts or other eye conditions.
F – Color Blindness
Color Blindness, a condition marked by difficulty distinguishing between certain colors, is often caused by an inherited genetic mutation affecting the photopigments in the cone cells responsible for color vision.
The most prevalent type is Red-Green Color Blindness, impacting approximately 8% of males and 0.5% of females of Northern European ancestry.
This particular form complicates the differentiation between shades of red and green.
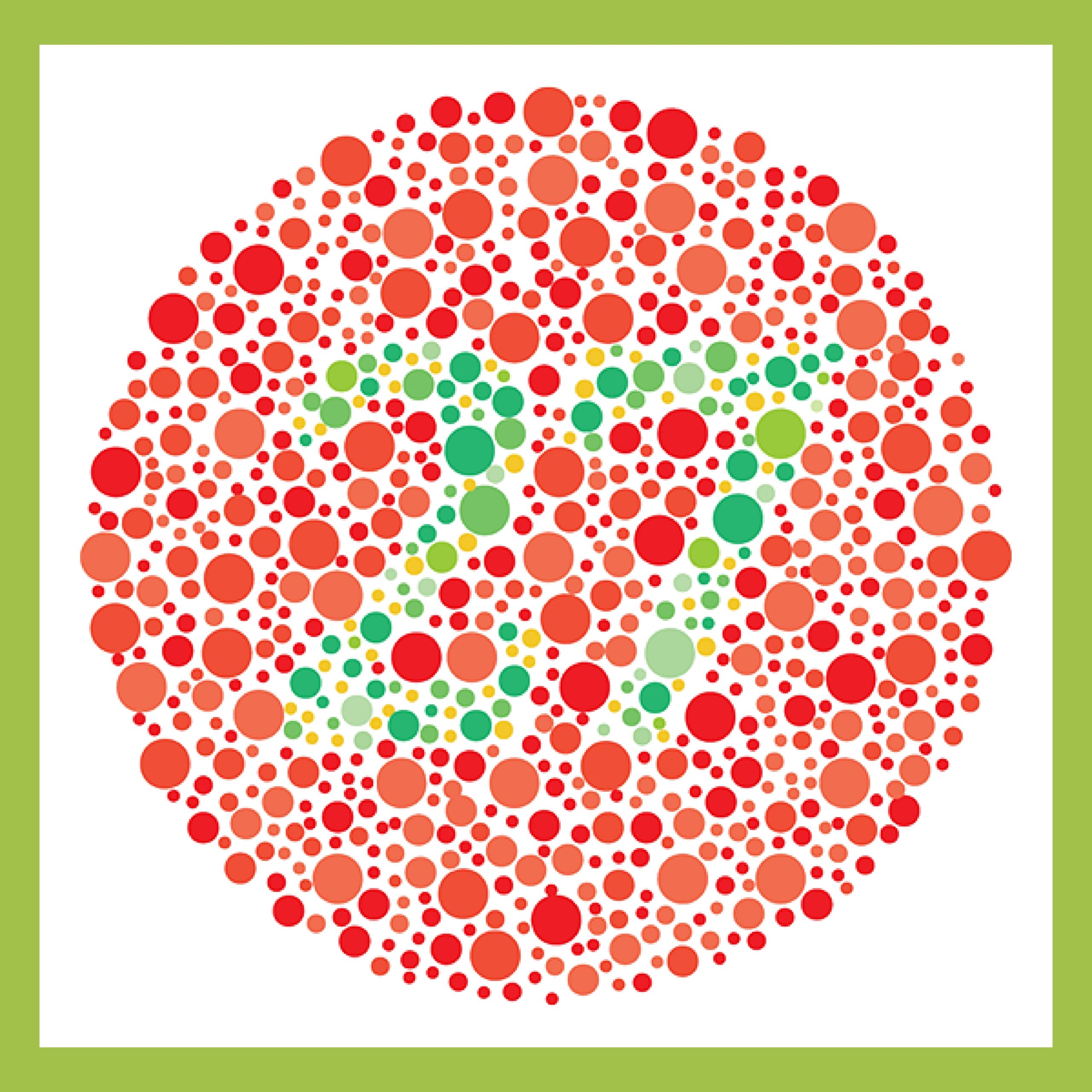
Other variants of Color Blindness include Blue-Yellow Color Blindness and the exceptionally rare Total Color Blindness.
Diagnosis typically involves tests using colored images or plates, requiring individuals to identify embedded shapes or numbers.
While there’s no cure for Color Blindness, various aids exist, including special lenses and glasses enhancing color perception, smartphone apps, and computer programs tailored for individuals with Color Blindness.
Although not considered a severe condition, Color Blindness can pose challenges in tasks requiring color vision, such as identifying traffic lights or interpreting color-coded graphs or maps.
Certain careers, like those of pilots or electricians, may also present difficulties for individuals with Color Blindness.
G – Conjonctivitis (Pink Eye)
Conjunctivitis, commonly known as Pink Eye, denotes inflammation of the conjunctiva, as previously discussed.
This condition can arise from viral or bacterial infections, allergies, or exposure to irritants like smoke or chemical fumes.
In some cases, blurred vision or light sensitivity may occur.

However, the hallmark symptoms of Conjunctivitis include redness and swelling of the conjunctiva, itching or burning sensations in the eyes, excessive tearing, and a discharge that may range from watery to thick, yellow, or green.
The approach to treating Conjunctivitis depends on its underlying cause.
Bacterial Conjunctivitis responds well to antibiotic eye drops or ointments, while Viral Conjunctivitis often resolves without specific treatment within a week or two.
Allergic Conjunctivitis can be managed with antihistamine eye drops or oral medications to alleviate inflammation and symptoms.
Preventive measures, such as frequent handwashing and avoiding the sharing of personal items, are crucial to curb the spread of Conjunctivitis.
Contact lens wearers are advised to abstain from using lenses until the infection clears, and any potentially contaminated lenses or cases should be discarded.
With diligent care and proper management, most instances of Conjunctivitis can be successfully treated, warning of long-term damage to the eyes.
H – Corneal Ulcers
Corneal Ulcers are open sores that develop on the Cornea, the transparent outer layer covering the Iris and Pupil of the eye.
These ulcers can result from bacterial, viral, or fungal infections, as well as injuries or prolonged contact lens wear.
Prominent symptoms of Corneal Ulcers include pain, redness, eye inflammation, sensitivity to light, blurred vision, and a discharge ranging from watery to thick, yellow, or green.
If left untreated, Corneal Ulcers pose the risk of corneal scarring and permanent vision loss. The approach to treating these ulcers hinges on the cause and the severity of the infection.
Bacterial ulcers respond well to antibiotic eye drops or ointments, while viral ulcers may require antiviral medications.
Fungal ulcers can be more challenging and may require oral or intravenous antifungal medications alongside topical treatments.
In severe cases where vision is significantly compromised, a Corneal Transplant might be considered, involving the removal of the damaged cornea and its replacement with a healthy donated cornea.
However, this intervention is typically reserved for extreme situations. Urgent treatment is imperative to prevent enduring damage to the eye and safeguard visual acuity.
I – Diabetic Retinopathy
Diabetic Retinopathy is a severe eye condition resulting from complications associated with diabetes.
Elevated blood sugar levels contribute to the damage of blood vessels in the Retina, the light-sensitive tissue at the back of the eye.
There are two primary types of Diabetic Retinopathy: Non-Proliferative Diabetic Retinopathy (NPDR) and Proliferative Diabetic Retinopathy (PDR).
In NPDR, in the early stage, damaged blood vessels in the Retina may leak fluid or blood, leading to swelling or the formation of deposits called exudates. Left untreated, this can result in blurred vision or vision loss.
In PDR, the advanced stage involves the growth of fragile new blood vessels in the Retina and vitreous gel of the eye. These vessels are prone to leaking blood, potentially causing scarring and the formation of scar tissues.
These scar tissues can exert traction on the Retina, potentially leading to detachment and permanent vision loss if not promptly addressed.
Prevention or slowing down of Diabetic Retinopathy is achievable through effective blood sugar control, regular eye exams, and early intervention.
Treatment options encompass laser surgery to seal leaking blood vessels, eye injections to reduce inflammation and leakage, and surgical procedures to remove scar tissue or reattach a detached retina.
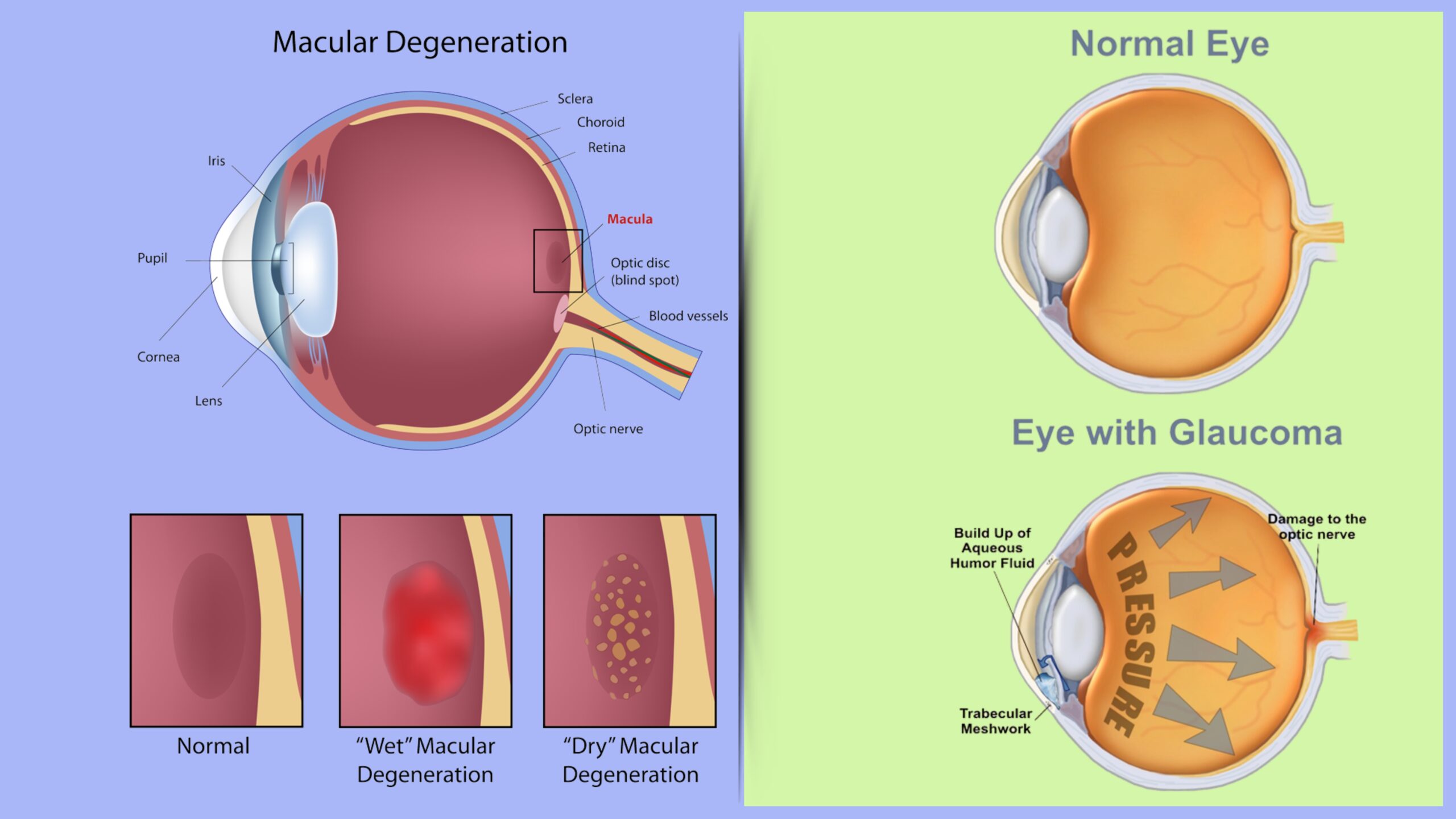
J – Glaucoma
Glaucoma encompasses a group of eye diseases that detrimentally affect the Optic Nerve, responsible for transmitting visual information to the brain.
Typically, this damage is instigated by an elevation in intraocular pressure (IOP) inside the eyeball.
Representing a leading cause of global blindness, Glaucoma can induce gradual and irreversible vision loss.
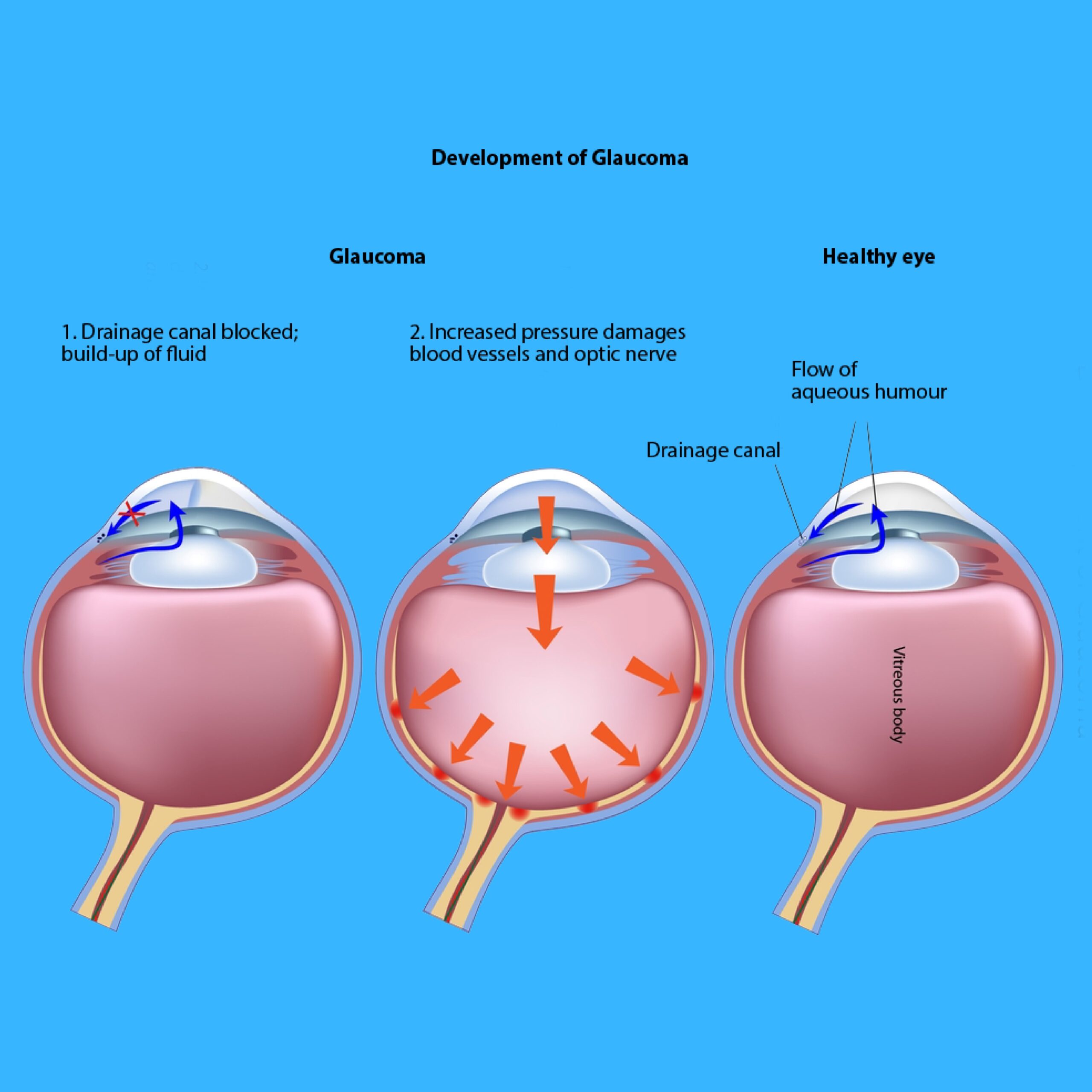
In its early stages, Glaucoma often manifests without noticeable symptoms, making vision loss potentially unnoticed until it reaches a severe stage.
Progression of the disease may lead to peripheral vision loss, challenges with night vision, and eventually central vision loss.
Various types of Glaucoma exist, with Open-Angle Glaucoma being the most prevalent, and Angle-Closure Glaucoma, while less common, is capable of causing a sudden and severe increase in IOP.
Additional types include Normal-Tension Glaucoma, occurring despite normal IOP levels, and Secondary Glaucoma, developing due to other eye conditions or medications.
Treatment objectives for Glaucoma involve reducing IOP to forestall further optic nerve damage. This can be achieved through the use of eye drops, oral medications, laser therapy, or surgery, contingent on the type and severity of Glaucoma.
Regular eye exams play a pivotal role in the early detection and treatment of Glaucoma, particularly for individuals at elevated risk, such as those with a family history or those over the age of 60.
K – Hyperopia or Hypermetropia
Hyperopia, commonly referred to as Farsightedness arises when the eye is too short or the cornea is too flat, causing light to converge behind the retina instead of directly on it.
This optical condition leads to challenges in clearly seeing objects up close, with distant objects appearing clearer.
People with hyperopia typically have eyeballs shorter than normal or corneas that are insufficiently curved, resulting in light focusing behind the retina.
Common symptoms of hyperopia include difficulty seeing nearby objects, eye strain, headaches, and fatigue, particularly after engaging in close work or reading.
However, individuals with mild hyperopia may not experience noticeable symptoms.
Correction for hyperopia is possible through eyeglasses or contact lenses designed to redirect light onto the retina.
Refractive surgeries like LASIK or PRK can also be viable options. In certain cases, treatment may not be necessary for mild hyperopia without accompanying symptoms.
Regular eye exams play a crucial role in early detection, including identifying hyperopia. While hyperopia can affect individuals of all ages, it is more prevalent in children and tends to diminish with age.
L – Iritis
Iritis, also recognized as Anterior Uveitis denotes inflammation affecting the iris, the colored part of the eye regulating the Pupil’s size.
This condition can be triggered by factors such as infection, autoimmune disorders, or eye trauma.
In severe instances, Iritis may lead to complications like Glaucoma or Cataracts, potentially resulting in permanent vision loss.
Common symptoms of Iritis encompass pain, redness, eye inflammation, sensitivity to light, blurred vision, and a small pupil unresponsive to changes in light.
The approach to treating Iritis is contingent upon the underlying causes and the inflammation’s severity. Topical corticosteroid eye drops are often prescribed to alleviate symptoms by reducing inflammation.
In more severe cases, or when an infection is the root cause, oral medications may be required to manage inflammation and avert complications.
Individuals experiencing symptoms of Iritis are urged to promptly schedule an eye exam with a healthcare professional. Timely treatment is crucial to prevent enduring damage to the eye and preserve optimal vision.
M – Keratitis
Keratitis, due to inflammation of the Cornea, the transparent outer layer covering the Iris and Pupil, can arise from bacterial, viral, or fungal infections, as well as injury or contact lens use.
Individuals with Keratitis may also experience sensations of a foreign body in the eye or excessive tearing. Key symptoms include pain, redness, eye inflammation, sensitivity to light, blurred vision, and eye discharge varying in consistency and color.
The approach to treating Keratitis is contingent upon the underlying causes and the infection’s severity.
Bacterial Keratitis typically responds to antibiotic eye drops or ointments, while Viral Keratitis may require antiviral medication.
Fungal Keratitis, more challenging to treat, may necessitate oral or intravenous antifungal medication in addition to topical treatments.
In severe cases where vision is significantly compromised, a corneal transplant may be considered, entailing the removal of the damaged cornea and its replacement with a healthy donated cornea.
However, this intervention is usually reserved for instances of substantial vision impairment.
Prompt treatment is crucial to prevent enduring damage to the eye and preserve vision, especially if detected through a comprehensive eye exam.
N – Lisch Nodule
Lisch Nodules are benign growths or bumps found on the Iris, typically yellow or brown in color and varying in size.
Characteristic of the genetic condition Neurofibromatosis type 1 (NF1), these nodules are a hallmark feature of this inherited disorder, which leads to the development of tumors on nerves throughout the body.
Notably, Lisch Nodules themselves rarely induce vision problems or noticeable symptoms and are often discovered during routine eye exams in individuals with NF1.

These eye exams play a crucial role in confirming NF1 diagnoses, particularly in cases where other apparent symptoms are absent.
While Lisch Nodules generally do not require specific treatment, individuals with NF1 are advised to undergo regular eye exams to monitor for potential changes or vision problems.
Additionally, comprehensive medical and supportive care may be necessary to manage other symptoms and complications associated with NF1.
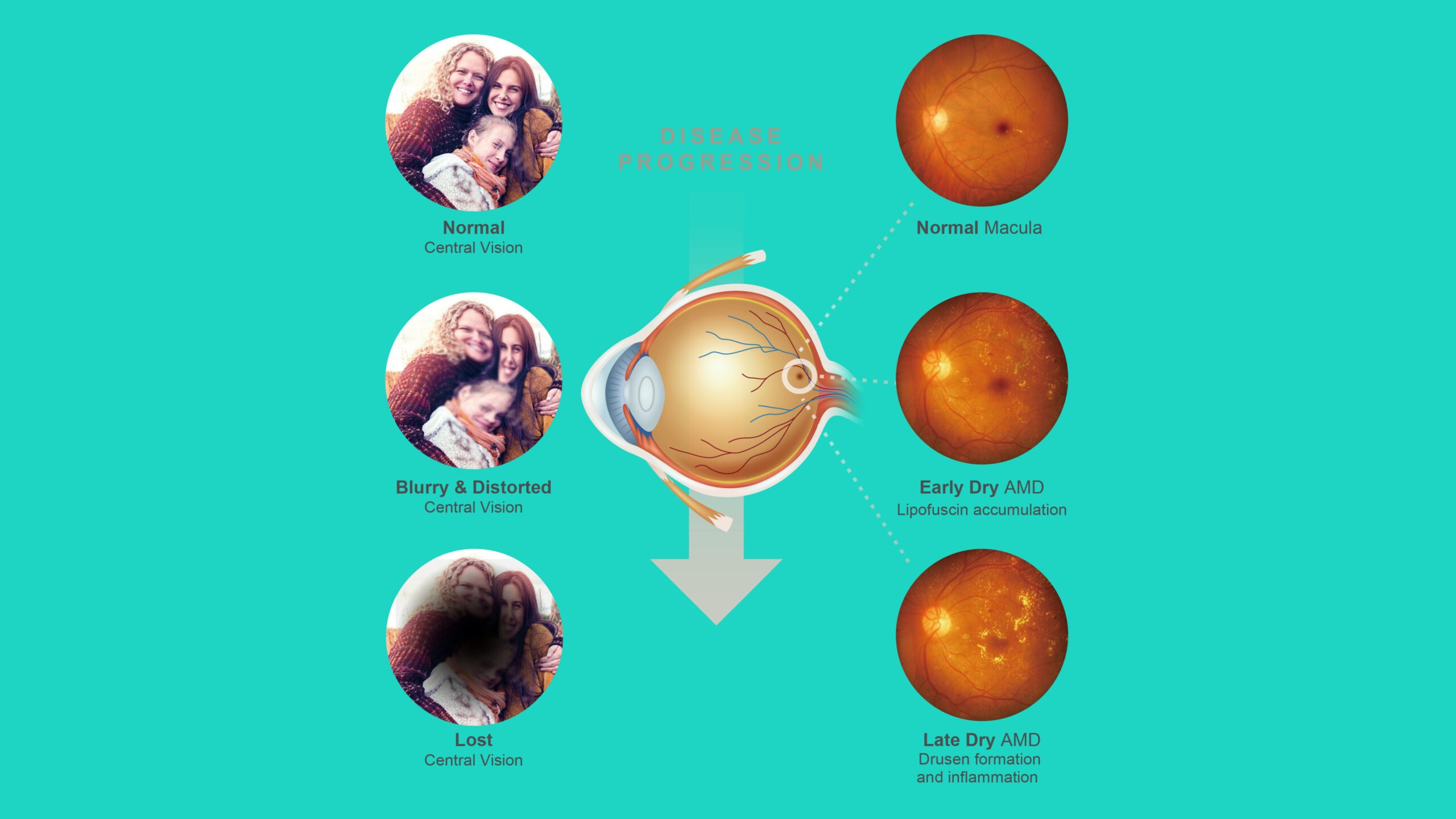
O – Macular Degeneration
Macular Degeneration, a prevalent eye condition, targets the Macula—integral for Central Vision.
This ailment encompasses two primary types:
01 – Dry Macular Degeneration: The most widespread form, constituting approximately 90% of cases. It unfolds as cells in the Macula degrade, leading to a gradual decline in light-sensitive cell functionality. Over time, this deterioration results in a progressive loss of Central Vision.
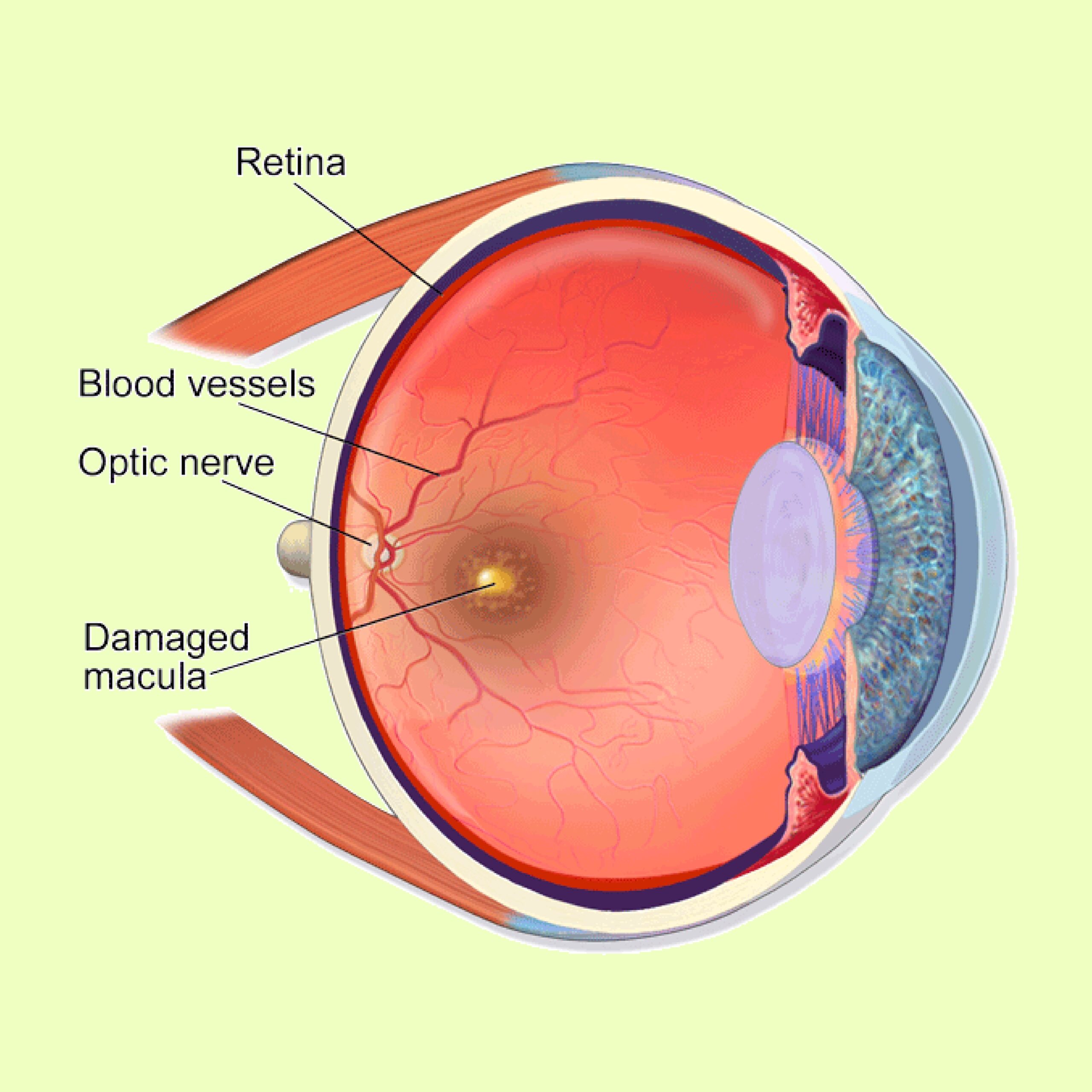
02 – Wet Macular Degeneration: Less prevalent but more severe, it arises when abnormal blood vessels develop beneath the retina, leaking fluid or blood and causing macular damage. This form precipitates rapid and severe Vision Loss.
While the precise causes of Macular Degeneration remain not entirely understood, a blend of genetic and environmental factors is implicated.
Age is a significant risk factor, with most diagnoses occurring in individuals over the age of 50.
Although no cure exists, various treatments—such as Medication Injections, Laser Therapy, and Photodynamic Therapy—can decelerate disease progression and preserve vision.
Embracing certain lifestyle modifications, such as quitting smoking and adopting an antioxidant-rich diet, may aid in reducing the risk or slowing the advancement of Macular Degeneration.
P – Myopia
Myopia, commonly known as Nearsightedness, manifests when the eye is excessively long or the cornea exhibits a steep curvature.
In such cases, light converges in front of the retina rather than precisely on it, resulting in challenges in seeing distant objects clearly.
This prevalent vision issue affects approximately 30% of the U.S. population, with a higher prevalence among individuals engaging in extensive close-up activities like reading or computer use.
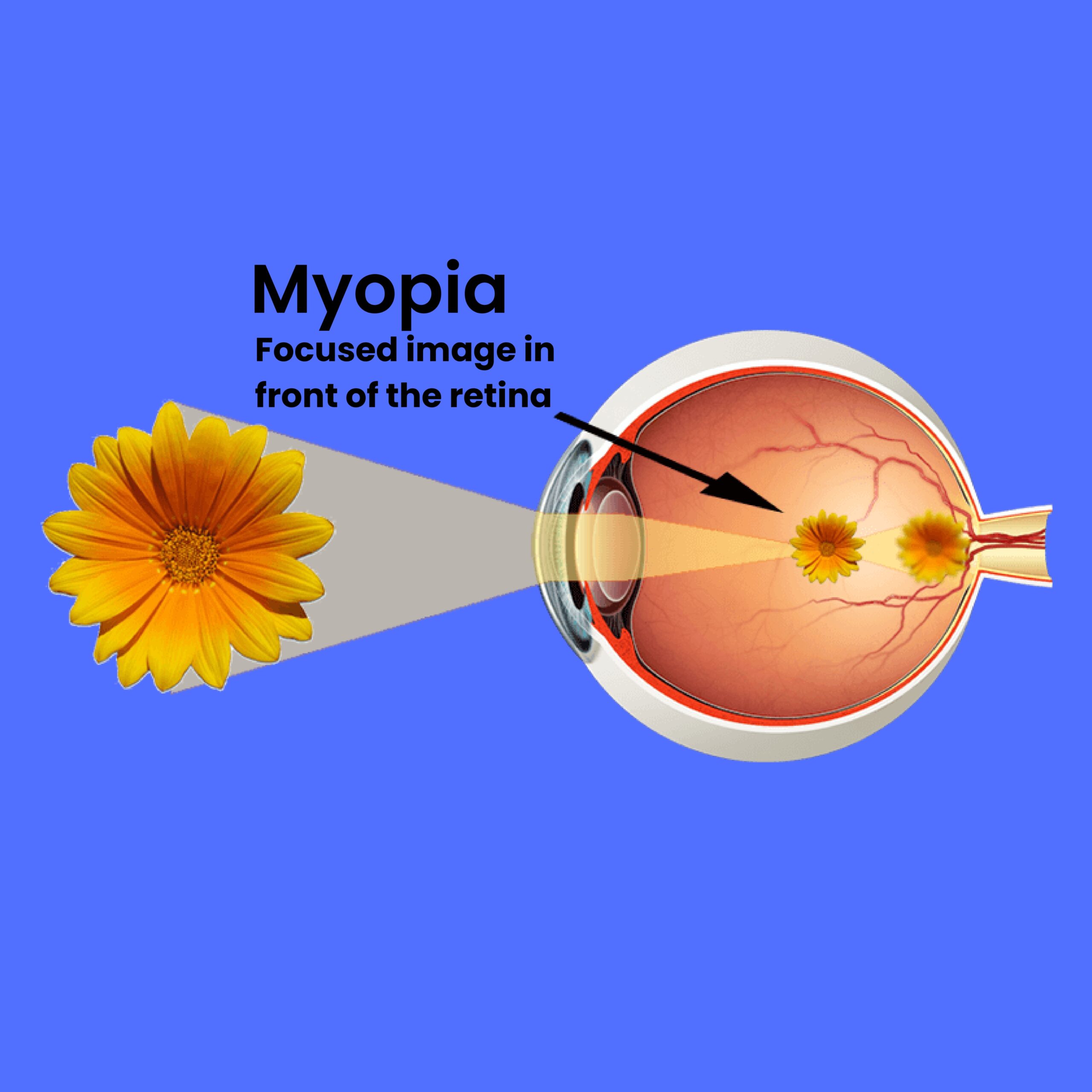
The symptoms of myopia encompass blurred vision, eyestrain, headaches, and the need to squint for clear vision of distant objects.
Typically emerging in childhood, myopia tends to progress until the age of 20-30 and can have a hereditary component. Diagnosis is accomplished through a comprehensive eye exam, including visual acuity and refraction tests.
Treatment options for myopia include corrective lenses, such as eyeglasses or contact lenses, redirecting light onto the retina for clearer vision. Refractive surgeries like LASIK offer an alternative for eligible candidates.
Emerging therapies, like Orthokeratology, involving overnight contact lens wear to reshape the cornea, and low-dose atropine eye drops, demonstrating efficacy in slowing myopia progression in children, show promise.
Regular eye exams are imperative to detect and address myopia early, as it can potentially lead to more serious eye conditions such as cataracts, glaucoma, and retinal detachment.
Q – Nyctalopia
Nyctalopia, commonly referred to as Night Blindness, characterizes a condition wherein individuals encounter difficulty seeing in low-light or dark environments.
This makes activities like night driving or navigating dimly lit spaces challenging.
Several factors contribute to Nyctalopia, including vitamin A deficiency, Retinitis Pigmentosa, Cataracts, and certain medications.
It can also serve as a symptom of underlying medical conditions like Diabetes or Liver Disease.
Treatment approaches for Nyctalopia hinge on identifying and addressing the root cause.
For instances linked to vitamin A deficiency, supplements or an increased intake of vitamin A-rich foods may be recommended.
Adjusting medications or opting for alternatives becomes crucial if medication usage contributes to the condition. Treating the underlying medical condition, such as Diabetes or Liver Disease, can improve Nyctalopia symptoms.
Additionally, specialized glasses or visual aids may be prescribed to enhance vision in low-light conditions.
Nyctalopia underscores the importance of comprehensive eye care, ensuring timely diagnosis and tailored interventions for an improved quality of vision in varied lighting scenarios.
R – Nystagmus
Nystagmus is an eye condition characterized by sudden repetitive, involuntary eye movements, which can manifest as side-to-side, up-and-down, or circular motions.
This phenomenon may be congenital, present from birth, or develop later in life due to factors like injury, disease, or medication.
Individuals with Nystagmus may experience vision-related challenges, including blurred vision, difficulty seeing in low light, and struggles with tracking moving objects.
Some may adopt a specific head position, known as a ‘Null Point,’ to mitigate the intensity of eye movements and enhance vision.
While there is no outright cure for Nystagmus, several treatments exist to address its impact.
These may include personalized eyeglasses prescriptions, contact lenses, and specific medications aimed at improving vision and mitigating the severity of eye movements.
Managing Nystagmus necessitates individualized approaches tailored to the unique circumstances of each case.
S – Presbyopia
Presbyopia, an age-related condition, impacts the eye’s ability to focus on near objects and is a common refractive error in individuals aged 40 and above.
This occurrence arises from the natural lens of the eye losing flexibility, diminishing its capacity to adapt to focusing on nearby objects.
Individuals experiencing Presbyopia may encounter challenges in reading small print or discerning close-up objects, often accompanied by eye strain or headaches during near-sighted activities.
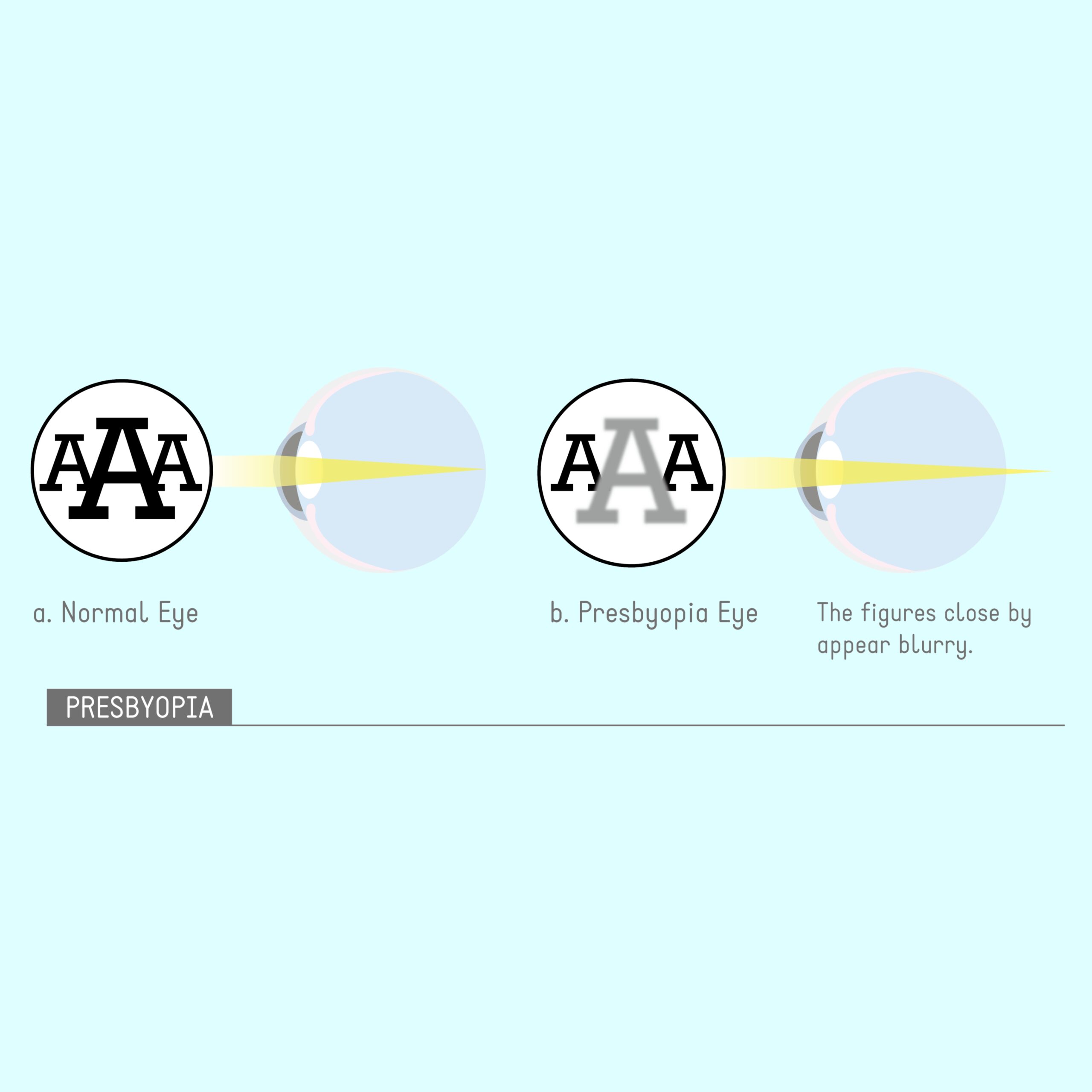
Recognized as a natural facet of aging, Presbyopia is nearly ubiquitous in older individuals.
Correction measures include reading glasses, bifocals, progressive lenses, or multifocal contact lenses. Refractive surgeries like LASIK also offer options for addressing Presbyopia.
Emphasizing the significance of regular eye exams, not only for Presbyopia management but also for monitoring and addressing potential additional eye conditions that may arise over time.
A proactive approach to eye health ensures timely detection and tailored interventions for a comprehensive and optimal vision experience.
T – Prosopometamorphopsia
Prosopometamorphopsia is a neurological condition categorized under Visual Agnosia, that perturbs the perception of faces, representing a group of disorders impacting visual recognition.
Prosopometamorphopsia individuals encounter distortions in facial feature perception, leading to challenges in recognizing and identifying faces.
These distortions may manifest as alterations in size, shape, or texture, creating difficulties in discerning familiar faces, including those of family members, friends, and colleagues.

Additionally, recognizing various emotions expressed on faces becomes challenging.
The origins of Prosopometamorphopsia lie in neurological conditions such as brain injury, stroke, or degenerative disorders like Alzheimer’s disease.
Treatment avenues encompass Visual Aids and Cognitive Therapies designed to enhance facial recognition skills and address underlying neurological conditions.
Understanding and addressing Prosopometamorphopsia entails a multidisciplinary approach tailored to individual circumstances for optimal outcomes.
U – Retinitis
Retinitis is a condition characterized by inflammation of the retina—the thin tissue at the back of the eye responsible for transmitting visual signals to the brain.—
Retinis can arise from various causes, including viral, bacterial, or parasitic infections, as well as autoimmune disorders.
Manifesting symptoms encompass decreased vision, blurred vision, floaters or spots in the visual field, and sensitivity to light.
Pain and redness in the eye can also occur in certain cases.
Effective treatment for Retinitis hinges on identifying the underlying cause and evaluating the severity of inflammation.
Antiviral, antibiotic, or antiparasitic medications may be prescribed for infection-related cases, while immunosuppressive medications may be employed for autoimmune disorders.
Timely intervention is critical, as untreated Retinitis holds the potential for permanent Vision Loss.
Individuals experiencing symptoms should promptly schedule an Eye Exam with an eye care professional to initiate swift and appropriate treatment, safeguarding the long-term health of the eye and preserving vision.
V – Stye
A Stye, also referred to as Hordeolum is a painful, red bump that emerges on the eyelid due to a bacterial infection affecting the Oil Glands.
Common symptoms include redness, swelling, tenderness, and light sensitivity, with some cases presenting discharge and a crusty buildup on the eyelid.
Management of a Stye typically involves warm compresses to facilitate drainage and healing.

Antibiotic ointments or drops may be prescribed to combat the infection. In instances where a Stye persists despite these measures, or if drainage is necessary, seeking assistance from an eye care professional is recommended.
Caution is advised against squeezing or popping a Stye, as this may spread the infection and pose potential complications.
If symptoms suggestive of a Stye are experienced, scheduling an Eye Exam with a professional is strongly recommended to determine the most effective course of treatment.
W – Uveitis
Uveitis is a condition characterized by inflammation of the Uvea—the eye’s middle layer encompassing the Iris, Ciliary Body, and Choroid.—
It can result from infections, autoimmune disorders, or eye trauma.
Symptoms often include pain, redness, eye inflammation, sensitivity to light, blurred vision, and the presence of floaters or spots in the visual field.
Some individuals with Uveitis may also manifest a non-responsive, small pupil under varying light conditions.
Effective treatment of Uveitis hinges on identifying the underlying causes and gauging the severity of inflammation.
Topical Corticosteroid eye drops are commonly prescribed to mitigate inflammation and alleviate symptoms.
In more severe instances, particularly those caused by infections, oral medications or injections may be necessary to control inflammation and avert complications.
Neglected or severe Uveitis cases pose risks of complications like Glaucoma, Cataracts, or permanent Vision Loss.
Given these potential consequences, it is crucial to promptly schedule an Eye Exam with an eye care professional upon experiencing Uveitis symptoms.
Timely intervention is vital for preventing lasting damage to the eye and preserving Eyesight.

IV – Eye Exams for Early Infection Detection
Eye Exams serve as crucial tools in the timely detection of various eye infections, which can range from mild to severe and result from bacteria, viruses, fungi, or parasites.
Common infections, as discussed earlier, encompass Conjunctivitis, Styes, Keratitis, and more.
An essential benefit of Eye Exams lies in their ability to identify infections early, often before significant damage occurs or affects other bodily regions.
During an Eye Exam, an optometrist or ophthalmologist employs various techniques and instruments to scrutinize the eye and adjacent tissues for infection signs.
Prominent indicators, like redness and inflammation of the conjunctiva, are thoroughly examined. Special dyes and blue light may be utilized to detect corneal abrasions or ulcers caused by bacterial or fungal infections.
Additional signs, such as vision changes, light sensitivity, or ocular discomfort, are also assessed.
Routine Eye Exams typically involve various procedures, tailored to individual needs and the examination purpose. Key components encompass:
01 – Medical History and Symptoms Assessment: Inquiry into prior eye conditions, surgeries, and current symptoms.
02 – Visual Acuity Test: Evaluates vision at different distances using an eye chart.
03 – Refractive Test: Determines the correct lens prescription for glasses or contact lenses.
04 – Eye Muscle Movement Test: Assesses eye alignment and movement.
05 – Slit Lamp Exam: Uses a specialized microscope to inspect the front of the eye, including the Cornea, Iris, and Lens.
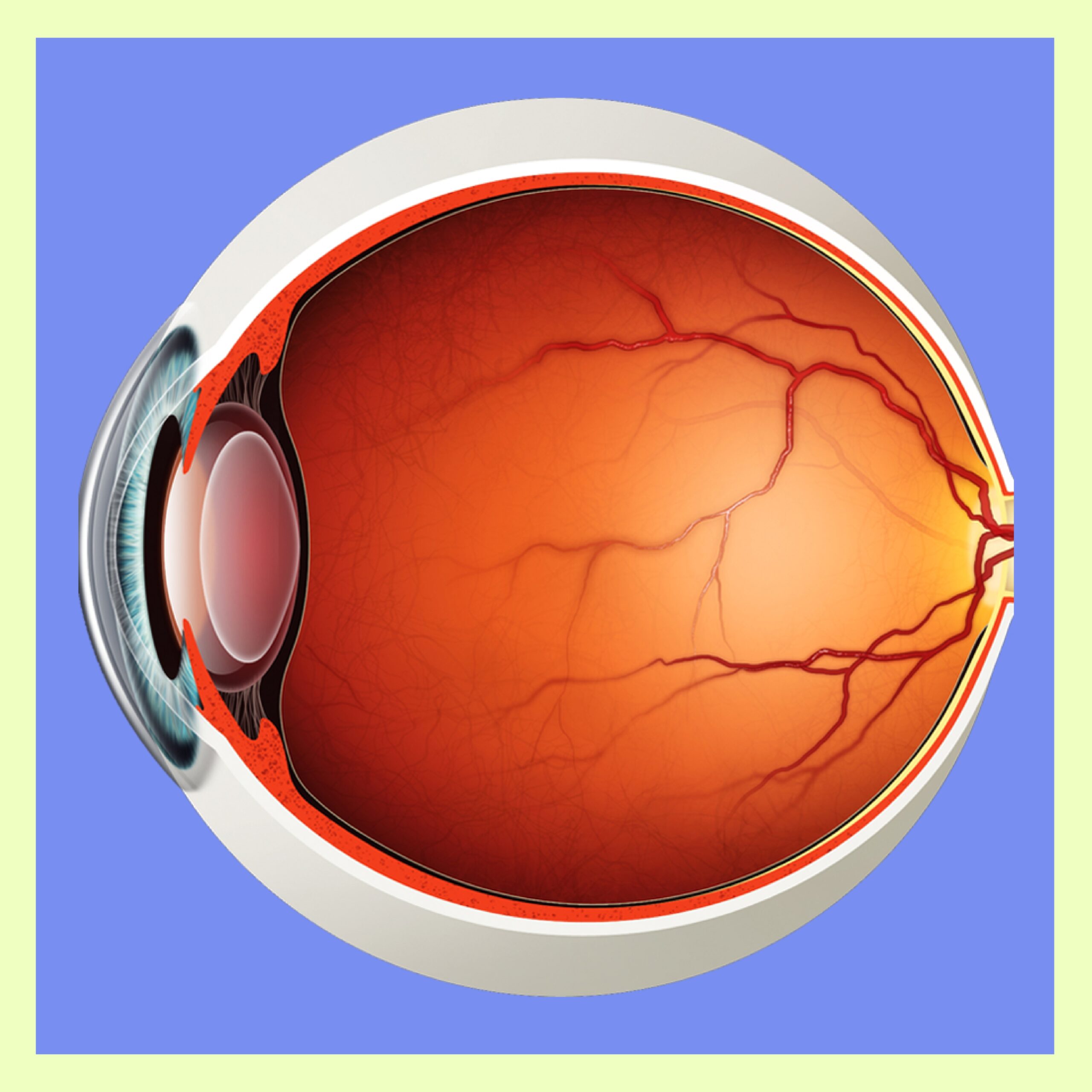
06 – Retinal Exam: Examines the back of the eye, including the Retina and Optic Nerve, utilizing instruments like an Ophthalmoscope or Retinal Camera.
07 – Intraocular Pressure Test: Measures eye pressure to detect conditions like Glaucoma.
Supplementary tests, such as Color Vision Testing, Visual Field Testing, or Special Imaging Tests, may be included based on individual requirements.
Timely detection through regular Eye Exams is paramount, as swift identification and treatment can avert complications.
Leaving an Eye Infection untreated can lead to Vision Loss, underscoring the importance of promptly seeking medical attention after detecting signs of infection.
V – Importance of Regular Eye Exams in Identifying Infections Early
Routine Eye Examinations are fundamental for maintaining optimal eye health and overall well-being.
Beyond identifying common refractive errors like Myopia (Nearsightedness), Hyperopia (Farsightedness), and Astigmatism, these exams play a crucial role in the early detection of various Eye Infections, even those lacking overt symptoms.
As explored earlier, Eye Infections can manifest across different eye structures, including the Cornea, Conjunctiva, and Eyelids.
Triggered by bacteria, viruses, fungi, or parasites, these infections can spread easily through contact with contaminated surfaces or fluids.
The significance of regular Eye Exams lies in their ability to uncover subtle or asymptomatic Eye Infections that might result from exposure to contaminated surfaces.
Detecting such infections promptly is paramount as it allows for early intervention before substantial damage occurs or potentially impacts other parts of the body.
One primary advantage of regular Eye Exams is the early identification of Eye Infections, enabling timely treatment with prescription eye drops or ointments.
This non-invasive approach is more manageable compared to situations where surgical intervention becomes necessary.
Moreover, early detection is crucial in preventing rare instances where certain eye infections pose life-threatening risks.
Individuals experiencing any symptoms of an Eye Infection or harboring concerns about their Eye Health are strongly encouraged to promptly schedule an Eye Exam with a qualified eye care professional.
Proactive measures contribute to the effective management of potential issues and ensure the preservation of both eye health and overall well-being.

VI – Why Ignoring Eye Infection Symptoms is Risky?
Imagine this colorful Universe you are accustomed to, which is always on the verge of meeting your sight every day before you wake up, and all of a sudden disappears.
It hasn’t disappeared because it really has vanished away, but because you become unable to see it again. How might the aftermath and feelings be with that situation, I prefer to leave you alone with its thoughts.
Eye infections can cause serious complications if left untreated, such as scarring, vision loss, and even blindness.
Symptoms like redness, swelling, sensitivity to light, and discharge are all signs that your eye may be infected and need immediate medical attention.
Ignoring these symptoms may lead to permanent damage to your eyesight so it is important to seek treatment as soon as possible.

VII – Comprehensive Preventive Measures for Optimal Eye Health
Ensuring optimal eye health involves adopting proactive measures to prevent potential issues and maintain clear vision.
From practicing good hygiene habits to avoiding potential sources of infection and prioritizing regular eye check-ups, comprehensive preventive measures play a crucial role in safeguarding your eyes.
This overview highlights key practices that contribute to long-term eye health and early detection of any emerging concerns.
A – Hygiene Practices for Eye Health
Maintain meticulous hygiene habits to safeguard your eyes. Wash your hands regularly to minimize the risk of transferring harmful bacteria or viruses to your eyes.
Avoid touching your eyes with unwashed hands to prevent potential infections.
Avoid sharing eye makeup, contact lenses, and other items that come into contact with the eyes with others. Replace your contact lenses and cases regularly.
B – Avoiding Potential Sources of Infection
Be proactive in steering clear of sources that could pose risks to your eye health.
Avoid rubbing your eyes, as this can spread infection. And avoid swimming in places with poor water quality.
Protect your eyes from irritants, such as smoke or harsh chemicals, and wear appropriate eye protection in environments where eye injuries are possible.
Make sure you wear protective eyewear when outdoors or in dusty environments. Wear sunglasses to protect your eyes from the sun’s ultraviolet rays.
Wear glasses or safety goggles when working with hazardous materials. If you wear contact lenses, make sure to clean them properly and replace them regularly.
Practice caution to prevent foreign objects or debris from entering your eyes.
C – Regular Eye Check-ups and Screenings
Prioritize routine eye check-ups and screenings as essential components of proactive eye care.
Regular examinations help detect refractive errors, eye conditions, or infections in their early stages, enabling timely intervention.
Stay proactive about your eye health by scheduling regular appointments with an eye care professional to ensure comprehensive and preventive care

VIII – Various Treatment Options for Eye Infections
Effective management of an eye infection involves tailored treatments based on the infection’s underlying cause and severity.
The following approaches may be recommended:
01 – Antibiotic, Antifungal, or Antiviral Medications:
Topical eye drops or ointments.
Oral antibiotics, antifungals, or antivirals for systemic infections.
02 – Steroid Eye Drops:
Prescribed to reduce inflammation in certain cases.
03 – Warm Compresses and Lubricating Eye Drops:
Utilized to alleviate swelling and soothe the eyes.
04 – Eyeglasses or Contact Lenses:
Recommended to minimize eye strain.
05 – Surgical Intervention:
Considered if the infection requires removal or drainage.
06 – Topical Ointments, Anti-Inflammatory, or Eye Patches:
As prescribed by the eye doctor for specific conditions.
07 – Home Remedies:
Cool compresses or tea bags for additional relief.
08 – Over-the-Counter Artificial Tears:
To alleviate discomfort and irritation.
Remember, seeking prompt medical attention is crucial to prevent complications like vision loss. If you suspect an eye infection, consult with your eye care professional for an appropriate diagnosis and tailored treatment.

IX – Enhancing Your Eye Health: Accessible Resources and Recommended Tools
A – Links to Reputable Sources for Further Information
American Academy of Ophthalmology (AAO): A leading authority on eye health, the AAO provides comprehensive resources covering various eye conditions, treatments, and preventive measures. Explore here.
National Eye Institute (NEI): Operated by the National Institutes of Health, NEI offers valuable insights into eye research, diseases, and vision-related topics. Discover more.
Optometry Times: A reliable source for up-to-date information on optometry and eye care, offering insights from industry experts. Access the site.
B – Recommended Eye Care Products and Tools
Preservative-Free Artificial Tears: Keeping your eyes lubricated is crucial for comfort and health. Opt for preservative-free artificial tears, such as Systane Ultra or Refresh Optive.
Blue Light Blocking Glasses: In our digital age, protect your eyes from prolonged screen exposure with blue light-blocking glasses. Brands like Gunnar and Felix Gray offer effective options.
Optometrist-Approved Supplements: Consider supplements like Omega-3 fatty acids and lutein, known for promoting eye health. Brands like Nature’s Bounty and EyePromise provide reputable options.
Eye Health Apps: Explore apps like EyeReader and EyeCare 20-20 to promote eye exercises and monitor screen time.
Also check out Sight Care, a natural, effective solution to fight eye infections and keep your eyes healthy. Click the link below to learn more about Sight Care:
Natural Supplement that Supports a Healthy Vision
By leveraging these resources and incorporating recommended products into your routine, you empower yourself to proactively care for your eyes and enhance your overall eye health.

Conclusion
Prioritizing Eye Health: Recognizing and Addressing Infections
Understanding the signs of an eye infection is paramount for maintaining optimal eye health and preventing potential complications.
Whether you notice redness, swelling, discharge, changes in vision, or discomfort in or around your eyes, it is crucial to treat these symptoms seriously and promptly seek the expertise of a qualified eye care professional.
If you harbor any concerns or queries regarding your eye health, it is advisable to consult with your eye care professional.
They will swiftly diagnose and initiate appropriate treatment for any eye infections. Disregarding signs of eye infections can lead to more severe vision problems and should never be underestimated.
Beyond seeking medical treatment, several preventive measures can also be adopted to reduce the risk of eye infections.
Regular handwashing, avoiding eye touching, refraining from sharing personal items like towels and makeup, and wearing protective eyewear when necessary all contribute to maintaining eye health.
Always remember, your eyes are precious and merit the utmost care. By staying informed and proactive about your eye health, you play a vital role in preventing eye infections and safeguarding your vision for the long term.
Table of Contents
Share this Post!
Sharing information about Eye Infections and Issues can indeed help others who are dealing with these eye conditions. Your efforts to spread awareness and knowledge can make a positive impact on someone’s life.
So, if you found this post helpful and think it can help others, please share it and feel free to do so.
Many people have eye problems and discomfort, and sharing this post might make a difference in their lives, even if you don’t know them personally.
Thank you for your time!